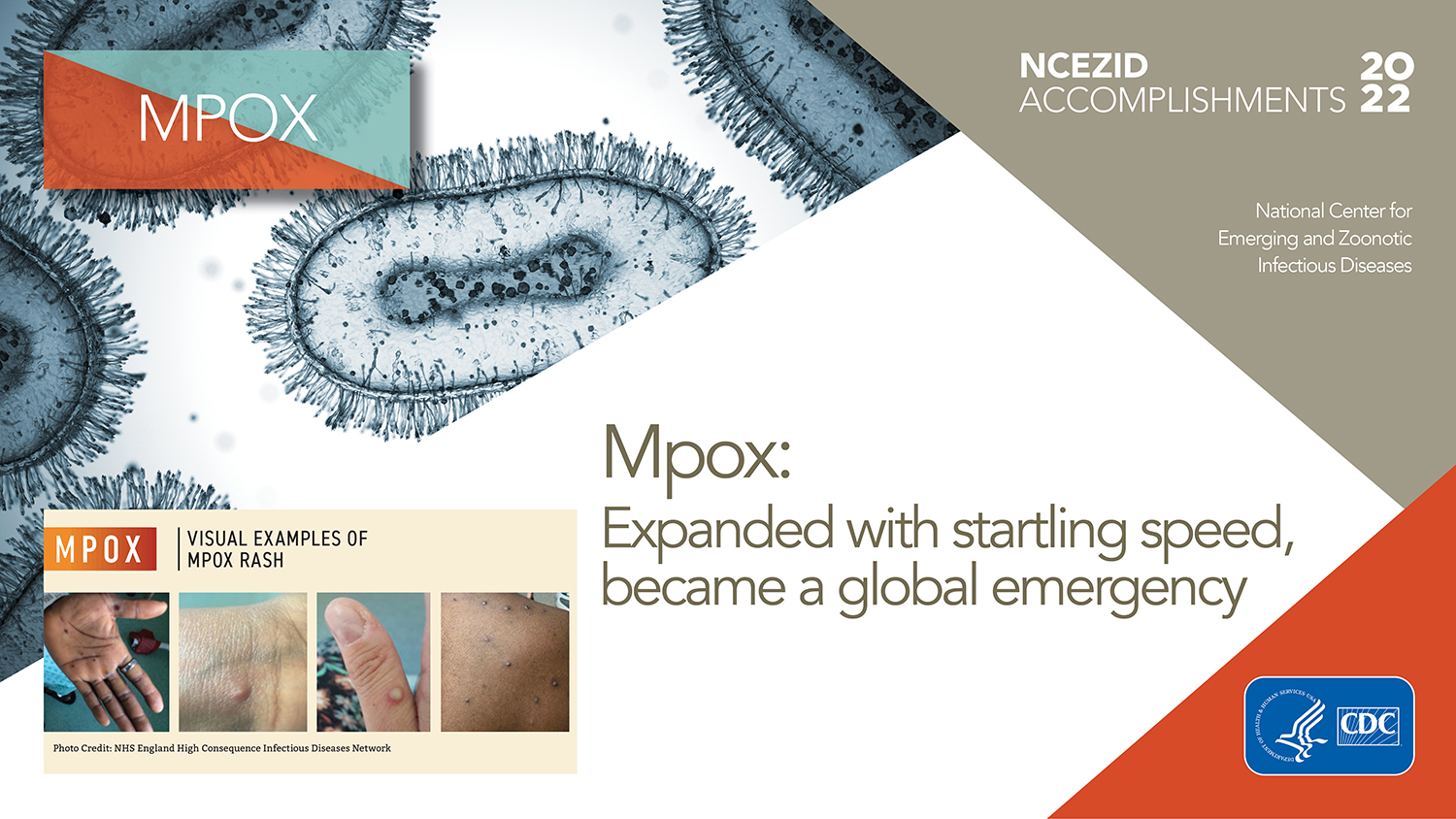
Mpox
Expanded with startling speed, became a global emergency
During 2022, partners and teams from CDC’s National Center for Emerging and Zoonotic Infectious Diseases (NCEZID) and from across CDC worked tirelessly to contain the spread of mpox in the United States. Following the first reported case in mid-May, the U.S. outbreak eventually swelled to roughly 30,000 cases and 20 total deaths in 2022. Although the outbreak presented new challenges, we were ready with decades of experience studying poxviruses and responding to global outbreaks.
Within months of the first U.S. case, global cases soared in more than 100 countries—including cases in nearly every U.S. state—making it the largest mpox outbreak in history. This led the World Health Organization and the U.S. Department of Health and Human Services to declare mpox a public health emergency. CDC’s efforts—with NCEZID experts at all levels of the response—intensified into August of 2022, after which case counts began declining.
Leading the response
CDC’s efforts against mpox long preceded the 2022 outbreak. Thanks to a long-term focus on preparedness and poxvirus research, clinicians and patients had reliable, validated assays to test for poxviruses and a better vaccine to prevent mpox with fewer side effects. Moreover, CDC was able to quickly detect and activate emergency response functions.
The mpox emergency response also drove home the power of partnerships. NCEZID and CDC colleagues provided strong leadership across all facets of the response, while working closely with partner organizations and health departments across the country. The 2022 outbreak disproportionately affected gay, bisexual, and other men who have sex with men. Community organizations, including partners in the LGBTQ+ community, played a critical role in raising awareness about the outbreak and sharing accurate information about vaccination and other ways people can protect themselves and prevent the spread of mpox.
As the response evolved, CDC provided technical assistance and guidance to health departments and clinicians, provided outreach to groups most affected by the outbreak, and facilitated access to vaccines and therapeutics. This global emergency underscored the many ways CDC, state and local health departments, and community-based organizations can effectively respond to evolving diseases together.

Jennifer McQuiston, DVM (CAPT, USPHS), who served as Response Incident Manager during the early months of the mpox outbreak, analyzes the latest case counts with Hilary Kelly, MPH, Chief of Staff for the response in CDC’s Emergency Operations Center. Partners have been essential during this emergency response, she said. “I want to thank the many healthcare providers, state and local public health officials, and community-based organizations, especially trusted messengers in the LGBTQ+ community, for their partnership to educate and protect those at greatest risk for mpox.”
Preparedness pays off
For years, NCEZID focused on improving the nation’s preparedness for public health emergencies caused by biothreats like anthrax, plague, and smallpox. This preparedness paid off. In 2005, NCEZID’s laboratory response experts partnered with leading poxvirus scientists to equip the Laboratory Response Network (LRN) with an FDA-cleared laboratory test that can detect non-variola orthopoxviruses, the family of viruses that includes mpox. CDC’s LRN consists of more than 110 laboratories across the country that can respond quickly to biological and chemical threats and other public health emergencies. Those steps to strengthen preparedness 17 years ago resulted in the LRN’s detection of the first mpox case in the United States on May 17, 2022. It also meant LRN laboratories across the network were equipped on day one of the outbreak with tests that provided actionable results to public health officials and clinicians.

Photo Credit: NHS England High Consequence Infectious Diseases Network
As mpox cases increased, NCEZID and other CDC scientists worked rapidly with FDA to expand testing through large commercial laboratories. In combination with LRN laboratories, this increased nationwide access and capacity to approximately 80,000 tests per week. These actions made it easier for clinicians to diagnose patients with mpox, which enabled timely isolation and treatment, vaccinations, and other public health actions to prevent the spread of disease. Continued efforts to strengthen the nation’s public health infrastructure, including public health laboratories, are critical to ensure the nation can rapidly respond to outbreaks of emerging infectious diseases and other public health emergencies.
Assisting travelers
NCEZID’s global migration expertise served a crucial role in the mpox response. NCEZID coordinated aircraft contact investigations by identifying travelers exposed to a person with mpox on arriving international flights, or flights between states, and sharing their contact information with health departments for notification and public health management. These experts also responded to notifications from other countries under the International Health Regulation regarding travelers with mpox who entered the United States. NCEZID informed travelers about how to protect themselves and others from mpox and what to do if they were exposed during travel. Experts also provided clinicians and health departments guidance on risk assessment and public health management of mpox cases and contacts in travel settings. We also collaborated with GeoSentinel, a worldwide network of travel medicine clinics, to conduct mpox surveillance so we can better understand how and where mpox spreads, who is most affected, and how to protect people from infection. NCEZID’s global migration capabilities serve a critical, specialized mission in CDC emergency responses, including the U.S. mpox response. As global migration responsibilities continue to rise, so does the need for expanded public health defenses to mitigate the risk of communicable disease spreading into and within the United States.