Our Work: 2020
Our Work - 2020

CDC, with federal and state partners, is investigating several multistate foodborne and animal-contact outbreaks, including the following:
- Two outbreaks of coli O157:H7 infections from undetermined sources; the strains of E. coli that are causing these outbreaks have previously been associated with leafy greens. One outbreak involves 21 cases in eight states, with eight hospitalizations and one death. The other involves 39 cases from 18 states, with 19 hospitalizations and no deaths. Public health officials are interviewing ill people, and FDA is conducting farm inspections, sampling, and traceback investigations.
- A third outbreak of E. coli infections that includes 12 cases from six states, with five hospitalizations and no deaths. The source of the outbreak has not been determined. Laboratory testing did identify the outbreak strain in a sample of Tanimura & Antle romaine lettuce in a single-head package. The investigation is ongoing to determine whether additional products may be contaminated with the outbreak strain of E. coli.
- Listeria monocytogenes infections linked to deli meats. Three states have reported 10 cases; all 10 people were hospitalized, and one has died. The investigation is ongoing to identify a specific type or brand of deli meat linked to illness. People who are at higher risk for getting sick with Listeria should avoid eating deli meats, unless they have been heated to an internal temperature of 165°F or until steaming hot just before serving.
- Salmonella infections linked to backyard poultry. This year so far, a record number of illnesses (over 1,659) have been reported from all 50 states; 326 people have been hospitalized, and one person has died. Stay healthy around your backyard flock by washing your hands, keeping your birds outdoors, and supervising young children around your flock.
- Salmonella infections linked to pet hedgehogs. CDC is collaborating with Canada to investigate. In the United States, 20 states have reported 41 cases, with eight hospitalizations and no deaths. The hedgehog source has not yet been identified.
November 18 marked 42 days, or two incubation periods, since the last survivor in Equateur Province, Democratic Republic of the Congo (DRC) tested negative for Ebola. Upon reaching this milestone, the DRC Ministry of Health (MOH) and the World Health Organization declared the outbreak over. The outbreak, which was announced on June 1 of this year, resulted in 130 cases and 55 deaths across 13 health zones. Because cases of Ebola due to sexual transmission or relapse are possible after an outbreak ends, public health officials must maintain enhanced surveillance and other activities to ensure that they quickly detect and respond to any new cases. CDC will continue to support the DRC MOH during this post-outbreak period.

This month, CDC promoted US Antibiotic Awareness Week (USAAW) (November 18-24) and C. diff Awareness Month. USAAW helps raise awareness about appropriate antibiotic use and the threat of antibiotic resistance across a One Health spectrum. For USAAW, CDC shared new data on antibiotic use, antibiotic resistance, and COVID-19 [PDF – 24 pages]; CDC’s Antibiotic Use Report: 2020 Update; and the newly released National Healthcare Safety Network (NHSN) AU Option Data Report. CDC staff presented on the CDC/Health Resources and Services Administration webinar “Implementation of Antibiotic Stewardship Activities in Critical Access Hospitals,” and provided remarks at the C. diff Foundation Patient and Family Symposium on C. diff prevention and antibiotic awareness on November 23. For C. diff Awareness Month, CDC’s C. diff webpages and materials were updated.
AMD Hackathon co-hosts Kelsey Florek (Wisconsin State Laboratory of Hygiene) and Logan Fink (Virginia Division of Consolidated Laboratory Services) announce the event's winners.
November’s session of AMD Virtual featured talks on modeling genomic data and a panel discussing state perspectives on using COVID-19 sequencing data. The conference also allowed users to register as teams for the first-ever AMD Hackathon: A Bioinformatics Scavenger Hunt. Participants received 10 bioinformatics-related questions over the course of a week, with each answer providing a clue that would be necessary to answer the final question. On November 20, members of Team UFC (Sarah Schmedes, Erin Young, Taj Azarian, Molly Hetherington-Rauth, and Tara Gallagher, all from outside CDC) were crowned winners of the Hackathon.
You can still register for the upcoming months of AMD Virtual. And once you register, you’ll also be able to access the archived recordings from October’s and November’s talks. AMD Virtual will begin again in January and continue its monthly sessions through April 2021.
CDC launches Project Firstline

Last month, CDC launched Project Firstline, a national infection control training collaborative, to address the gaps in healthcare infection control that have been underscored by the COVID-19 pandemic. Project Firstline will educate frontline healthcare workers about the rationale behind CDC’s infection control guidance and provide an opportunity to engage directly with CDC experts.
Project Firstline is designed to meet frontline healthcare workers’ needs as identified by CDC staff through their time in the field and by healthcare workers themselves during 24 listening sessions that Project Firstline partners hosted this summer.
Project Firstline will release infection control training modules and tools this month and will continue to participate in a series of virtual events to address the needs highlighted by healthcare workers on the front lines of the COVID-19 pandemic.
CDC partners with Antibiotic Resistance (AR) experts for Anti-Microbial Resistance (AMR) & COVID-19 webinars
For a four-part webinar series—”AMR in the Light of COVID-19”—CDC partnered with leading antibiotic resistance experts to discuss how the COVID-19 pandemic could shape strategies for combating Antibiotic Resistance (AR) around the world. Topics included tracking difficult-to-treat infections; the critical role of preventing drug resistant infections; how diagnostic testing improves the use of antibiotics and stewardship; and the roles and responsibilities of governments, industry, and patients. CDC staff joined as featured panelists in “Prevention is Stronger than a Cure” and “Responding to Difficult-to-treat Infections: Role and Responsibilities of Governments, Researchers, Industry and Patients.”
CDC encourages people to wear a mask on public transportation
On October 19, CDC published a strong recommendation for the public to wear masks while using public transportation and at transportation hubs. Spread of the virus through travelers has led—and continues to lead—to interstate and international spread of COVID-19. Masks, when worn appropriately, can reduce the chances of getting and spreading COVID-19. Check out the recent CDC scientific brief on the benefits of wearing masks to protect others and yourself.
CDC issues Framework for Conditional Sailing Order
On October 30, CDC issued a Framework for Conditional Sailing Order for cruise ships operating or seeking to operate in US waters. This Order replaces the No Sail Order that had been in place since March 14 and introduces a phased approach to resuming passenger operations in a way that reduces the risk of spreading COVID-19. During the initial phases, cruise ship operators must demonstrate adherence to testing, quarantine and isolation, and social distancing requirements to protect crew members. Cruise ship operators must also build the onboard laboratory capacity needed to test crew and future passengers.
Travel Planner

As the COVID-19 pandemic evolves, state, local, tribal, and territorial governments are providing guidance to travelers to reduce the risk of spreading COVID-19. However, it can be difficult for travelers to find jurisdiction-specific COVID-19 advisories, restrictions, and requirements along their journey or at their final US destination. CDC created a website called Travel Planner to serve as a single location that travelers can search to find COVID-19 information for the communities along their route and at their destination. This website helps health departments share their COVID-19 policies and will also help ensure that travelers can make informed decisions, protect themselves, and reduce transmission before, during, and after travel.

CDC, with federal and state partners, is investigating several multistate foodborne and animal contact outbreaks, including the following:
- Salmonella Stanley infections linked to wood ear mushrooms. As of October 5, a total of 43 ill people have been reported from 10 states, with 4 hospitalizations.
- Three separate outbreaks of Salmonella infections linked to contact with animals (backyard poultry, pet bearded dragons, and pet hedgehogs). Interest in animal companionship has increased during the COVID-19 pandemic, which may be contributing to these outbreaks. Visit the Healthy Pets, Healthy People website before adding new animals to your household to pick the best fit for your family.
In related news, the outbreak of Salmonella Newport infections linked to onions is now over. A total of 1,127 illnesses were reported from 48 states, with 167 hospitalizations. Red onions from Thomson International, Inc., were the likely source of the outbreak. Thanks to tools like SEDRIC, CDC quickly managed the outbreak and coordinated a rapid response that likely prevented further illnesses.
The count to 42 days, or two incubation periods since the last patient tested negative for Ebola, is on for the response to the Ebola outbreak in the Democratic Republic of the Congo’s (DRC) Equateur Province. Although a few probable cases were validated during the month, no new cases have been detected so far in October. As of October 26, there were 130 cases and 55 deaths across 13 health zones. CDC remains committed to helping DRC’s Ministry of Health bring the outbreak to an end. CDC deployers in the field are providing technical assistance in epidemiology, lab, communication, infection prevention and control, social and behavioral science, and vaccine. With suspected cases identified in neighboring Republic of Congo, CDC sent deployers to assess and support preparedness and potential response efforts there.
This month, the US government released the National Action Plan for Combating Antibiotic-Resistant Bacteria, 2020-2025, presenting coordinated, strategic actions to change the course of antibiotic resistance (AR) and improve the health of Americans. CDC continues to lead the AR public health response across the One Health spectrum with activities in healthcare, food and farms, communities, and the environment at home and abroad. CDC’s goals include a global lab network, vaccine data platform, and doubling CDC’s AR investments in health departments. The national plan addresses threats outlined in CDC’s 2019 AR Threats Report and builds off the first National Action Plan [PDF – 63 pages] released in 2015. CDC’s Antibiotic Resistance Coordination and Strategy Unit coordinated the agency’s input in the plan’s development across three centers and six divisions. This input informed the Task Force on Combatting Antibiotic-Resistant Bacteria, a collaborative group that includes the Office of the Assistant Secretary for Planning and Evaluation, Department of Defense, HHS, CDC, and United States Department of Agriculture.
Global Handwashing Day, occurring on October 15 each year, raises awareness about the importance of handwashing with soap and water to prevent infectious diseases. In honor of the day, CDC published a report in the Morbidity and Mortality Weekly Report (MMWR) describing handwashing behaviors among US adults before and during the COVID-19 pandemic. CDC’s other communication efforts for the day included:
- A video, hosted by CDC Deputy Director Anne Schuchat, on the importance of keeping hands clean during the COVID-19 pandemic;
- Newly created social media graphics and messages;
- Partner outreach efforts; and
- A new frequently asked questions page.
In January, CDC identified seven prevention priorities to address some of the most pressing concerns among foodborne, waterborne, and fungal diseases: adoption of the Model Aquatic Health Code, aspergillosis and triazoles, cholera, Shiga toxin-producing E. coli and leafy greens, Salmonella and chicken, Salmonella and ground beef, and vibriosis and shellfish. CDC launched the first phase of its new Prevention Priorities website on October 15. Please visit the site to learn about the priorities.
Americans are at an increasing risk of vector-borne diseases, and the United States is not adequately prepared to respond to these threats. To address the growing threat to public health, CDC, five federal departments, and the Environmental Protection Agency developed a joint National Public Health Framework for the Prevention and Control of Vector-Borne Diseases in Humans. The framework details the federal government’s goals and strategic priorities to address vector-borne diseases and lays the foundation for developing and executing a full national strategy, as authorized by the Kay Hagan Tick Act of 2019, with oversight and coordination delegated to the Office of the Secretary in DHHS. The national strategy will build out the activities that track to the framework’s goals and strategic priorities.
On October 13, CDC’s Office of Advanced Molecular Detection announced their new and improved Infosite 2.0. This site helps users with account requests, event registration, high performance computing resources, helpdesk tickets, training resources, and more. The updated site brings in new features and functions for users including a responsive search bar, simplified forms, hover-over tooltips, and a quick-access menu. The site also features a new live chat feature that allows users to talk with a SCBS representative to help with issues from 9am to 5pm Eastern. To learn about these new features and more, take a video tour anytime.
Through its Antibiotic Resistance Solutions Initiative, CDC is awarding more than $77 million to health departments and research partners nationwide to fight bacterial and fungal infections that resist treatment with antibiotics. Many projects focus on stopping the spread of resistant diseases in our communities, a growing problem that CDC highlighted in the 2019 AR Threats Report [PDF – 150 pages]. New projects include improving testing for a resistant strain of gonorrhea, researching antibiotic-resistant germs in wastewater, and studying whether antibiotic resistance can contaminate livestock feed and pet treats. Read the project descriptions.

Tribal partners put tick collars on dogs during the drive-up RMSF prevention campaign.
Rocky Mountain spotted fever (RMSF) is a dangerous tickborne disease impacting some Arizona tribal communities at high rates. Since the RMSF epidemic began in 2003, CDC has been working with state, federal, and non-profit partners to support tribal RMSF prevention programs. Seasonal prevention efforts in some communities typically rely on week-long door-to-door campaigns to provide education and tick collars and to administer pesticide to homes. Due to the ongoing risk of COVID-19, however, this fall’s campaign needed some creative changes. In consultation with CDC staff, one highly affected community organized a drive-up campaign so that community members could access this essential public health service, while maintaining social distancing. During the five-day campaign, 525 dogs were treated.

CDC led promotion for Sepsis Awareness Month in September, which also marked the 3-year anniversary of CDC’s award-winning Get Ahead of Sepsis national educational effort. Sepsis is the body’s extreme response to an infection and is a life-threatening medical emergency. Get Ahead of Sepsis seeks to raise awareness among the public and healthcare professionals about the importance of preventing infections and the early recognition and timely treatment of sepsis.
In the Equateur Province of the Democratic Republic of the Congo (DRC), CDC continues to support the Ministry of Health’s efforts against an Ebola outbreak that began June 1, 2020. CDC teams have traveled to DRC to provide technical assistance, and about 4,000 pounds of lab equipment and supplies have been sent to establish a lab in the town of Ingende. As of September 27, 2020, health officials reported 124 having been infected with the virus, including 50 who died.
For the first time, CDC has reported on outbreaks of intestinal illness among people linked to contact with animals or animal surroundings. In 2017, 59 animal contact outbreaks caused 1,518 illnesses, 312 hospitalizations, and three deaths. The most common cause of these outbreaks were the parasite Cryptosporidium (21 outbreaks involving 158 people) and the bacteria Salmonella (18 outbreaks involving 1,237 people). The report’s data are from CDC’s Animal Contact Outbreak Surveillance System (ACOSS) and can be viewed on an outbreak data dashboard hosted by the National Outbreak Reporting System (NORS).
Keeping swab samples for COVID-19 tests fresh and viable
A virus sample on a nasal swab might spoil if it is not kept in a special liquid that keeps it fresh and viable during transport on its way from the nose to a COVID-19 testing lab. The liquid is called viral transport medium (VTM), and in the pandemic, supplies of VTM have run low. CDC has written instructions [PDF – 8 pages] for professionals to make VTM themselves, and many labs and hospitals have used the document to increase their supplies. Harvard University included the instructions in a scientific study about producing mass quantities of VTM, and the U.S. Department of Defense has hired the company Corning to manufacture VTM using the CDC document.
Supporting refugees in lowering their risk of getting COVID-19
Refugees who come to the United States often live and work in conditions that put them at risk of getting COVID-19. CDC has created a booklet that refugees can receive in their native language before arriving in the country. The booklet explains how to stay healthy during the COVID-19 pandemic.

CDC, with federal and state partners, is investigating several multistate foodborne outbreaks, including the following:
- Salmonella Newport infections linked to onions. As of August 31, there have been 1,012 illnesses from 47 states. One hundred thirty-six people have been hospitalized. Thomson International, Inc. has recalled red, white, yellow, and sweet onions. Many other companies have also recalled onions or foods made with onions, such as chicken salad. The investigation is ongoing to determine if other onions are linked to the outbreak.
- Salmonella infections linked to peaches. As of August 27, a total of 78 ill people have been reported from 12 states, including twenty-three hospitalizations and no deaths. Prima Wawona has recalled peaches sold individually and peaches sold in bags. Several other companies have also recalled peaches or foods made with them like peach salsa and pastries. The investigation is ongoing to determine if other peaches are linked to the outbreak.
- Salmonella infections linked to contact with backyard poultry. As of July 28, a total of 938 ill people have been reported from 48 states, with 151 hospitalizations and one death.
CDC continues to respond to the ongoing Ebola outbreak in Equateur Province, DRC. August saw a rapid increase of cases and affected health zones. As of August 31, there were 109 cases and 47 deaths across 11 health zones. CDC has deployed a small team to DRC to support response efforts. Additionally, transition work continues in eastern DRC following the end of that outbreak in June. In August, the rapid diagnostic testing program began in Beni. CDC also designed instructional materials and trainings for the RDT field teams.

On August 10, the Environmental Protection Agency (EPA) registered nootkatone, a new active ingredient that CDC discovered repels and kills ticks, mosquitoes, and a wide variety of other biting pests. Nootkatone can be found in small quantities in Alaskan yellow cedar trees and grapefruit skin and is already used extensively as a flavor ingredient. CDC’s work with licensed partner Evolva demonstrates that nootkatone effectively repels and kills mosquitoes and ticks at rates similar to products already on the market. The availability of a new and effective insecticide ingredient paves the way for manufacturers to develop nootkatone-based consumer products and adds another tool to combat insecticide-resistance. Commercial products using the ingredient could be available as early as 2022.
CDC launched a major update to the MicrobeNet online database. CDC and the Association of Public Health Laboratories created a new interactive training module to help users quickly find the information they need. Users can also access archived MALDI (matrix-assisted laser desorption ionization) databases, so labs will not have to revalidate their methods for CLIA (Clinical Laboratory Improvement Amendments) as often when CDC adds new updates. The MALDI database now includes access to Argentina’s ANLIS MALDI-TOF bacterial database, which improved the range of rare bacterial and fungal pathogens featured in MicrobeNet.
The refreshed website isn’t the only big change for MicrobeNet this year. Due to genomic analysis at NCBI and other institutions, over 1,000 species’ taxonomic names have changed, and this has introduced a major shift from historical to current nomenclature. All these updates will make MicrobeNet a more accurate source of information for its 2,700+ users, who represent 1,476 organizations worldwide.
Using CDC data to inform the COVID-19 response in nursing homes

CDC’s National Healthcare Safety Network (NHSN) is the nation’s most comprehensive and widely used system for healthcare quality measurement and improvement and has played an important role in the COVID-19 response in nursing homes. In April, CDC worked closely with CMS to implement an Interim Final Rule [PDF – 80 pages] to make COVID-19 reporting to NHSN mandatory for all nursing homes (approximately 15,400) in the country. Within weeks, CDC had enrolled more than 12,000 nursing homes in NHSN for the first time, and now more than 99% of nursing homes are reporting essential COVID-19 data on resident and staff cases and deaths to NHSN, as well as on PPE supplies and staffing shortages. The data are shared regularly in analytic reports across the government COVID-19 emergency response and have helped states make decisions needed to protect nursing home residents and staff. NHSN has been a crucial part of the COVID-19 response and continues to provide the first and only national lens into the burden of COVID-19 in nursing homes.
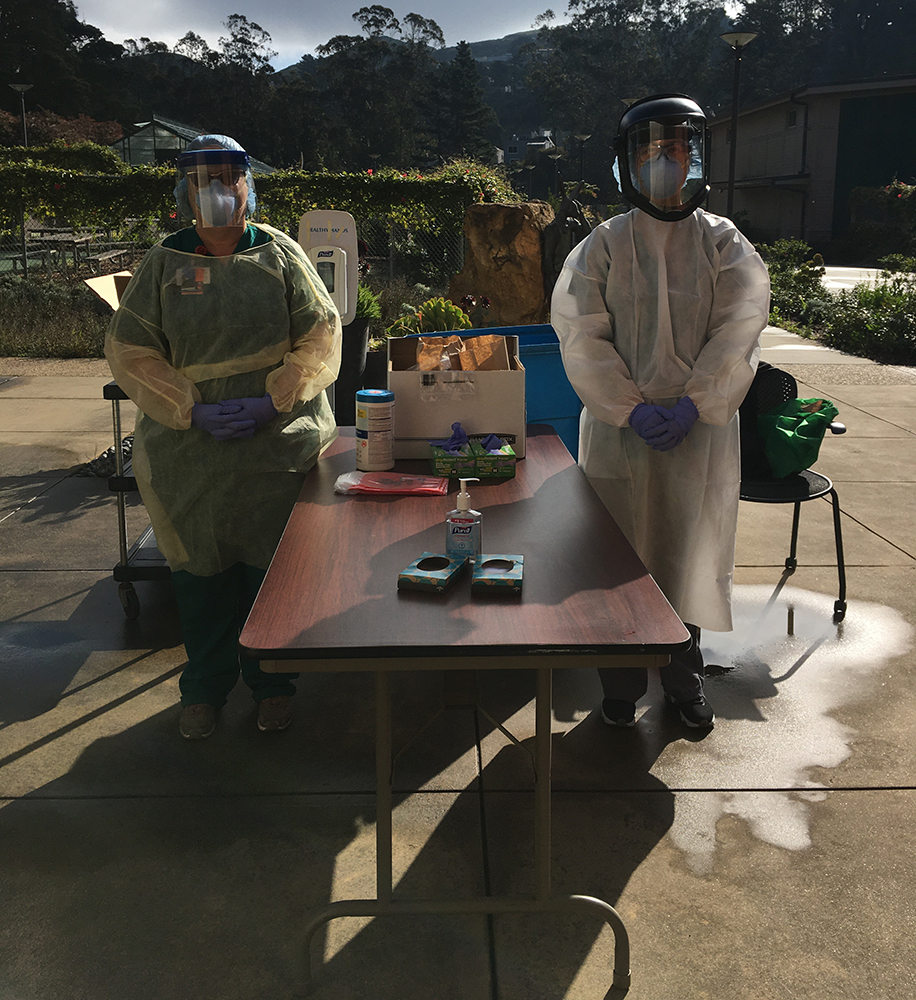
Responders support COVID-19 prevention work in San Francisco nursing home
In late March, San Francisco health officials recognized they needed to prevent further spread of COVID-19 in Laguna Honda Hospital and Rehabilitation Center, one of the largest nursing homes in the country. They asked CDC for help. Within 48 hours, CDC officials and epidemiologists deployed to Laguna Honda to provide infection control expertise.
The responders trained staff on proper infection control practices, how to optimize PPE, the process for creating an area to separate residents with confirmed COVID-19, and how to do contact tracing. Laguna Honda credits CDC and these collaborative efforts with helping them avert disaster and save lives. As of July 27, not one Laguna Honda resident or staff member had died of COVID-19. Details of this outstanding work are highlighted in a recent San Francisco Chronicle article.
CDC assists COVID-19 response efforts in Imperial County, California
In June, members from CDC’s US-Mexico Unit were deployed to Imperial County, California, a rural county on the US-Mexico border identified as a COVID-19 hotspot, to assist with data management, outbreak investigation, and contact tracing. Deployers faced a unique binational environment and a language barrier. Bilingual deployers proved to be invaluable, as Imperial County has a large population of Spanish speakers. Despite the 114˚F weather, the group’s hard work made a vital difference in protecting the health of a U.S. community along the border.
COVID-19 Travel Health Notice de-escalation

CDC’s Travelers’ Health regularly posts Travel Health Notices to notify travelers and others about health risks around the world. In March, CDC issued a Global Level 3 Travel Health Notice, notifying travelers about COVID-19 and encouraging them to avoid all nonessential international travel. In early August, CDC replaced the Global Notice with destination-specific COVID-19 risk assessments and travel recommendations for countries and U.S. territories. Learn how CDC determines the level of a destination’s COVID-19 Travel Health Notice.
CDC’s Arctic Investigations Program joins the state of Alaska in responding to COVID-19
CDC’s Arctic Investigations Program (AIP) has had a long-standing, close relationship with Alaska’s Department of Health and Social Services. When cases of COVID-19 began to be reported in Alaska, the state called on its CDC colleagues for help. Since the spring, CDC’s epidemiologists have helped the state investigate COVID-19 cases and contacts. From mid-May to early August, CDC’s laboratory staff worked onsite at the Alaska state public health laboratory, helping test tens of thousands of samples for COVID-19. CDC’s scientists will keep working alongside the state health department staff as the COVID-19 response continues.
Epidemiology and Laboratory Capacity (ELC) Cooperative Agreement provides unprecedented COVID-19 funding
The Epidemiology and Laboratory Capacity for Prevention and Control of Emerging Infectious Diseases (ELC) Cooperative Agreement has awarded $11 billion to state, local, and territorial health departments to support COVID-19 response efforts. In addition to processing these funding packages at a record pace, the ELC team remains committed to providing excellent customer service to all recipients.
CDC is investigating multiple outbreaks of Salmonella infections linked to contact with backyard poultry. There have been 938 sick people reported from 48 states. One hundred fifty-one people have been hospitalized and one death has been reported. About one-third of infections are among children younger than 5 years of age. Last year had the highest number of illnesses linked to backyard poultry, and this year is on track to exceed that number.

CDC and FDA are working with multiple state health departments to investigate a rapidly growing outbreak of Salmonella Newport infections. As of August 3rd, a total of 396 cases, including 59 hospitalizations, had been identified in 34 states. The source of the outbreak has been identified as onions. Thomson International, Inc. recalled red, white, yellow, and sweet yellow onions. The investigation is ongoing to determine if other onions are linked to the outbreak. Do not eat, serve, or sell recalled onions or products made with these onions.
CDC is responding to the Ebola outbreak in the Equateur Province of the Democratic Republic of the Congo (DRC). As of July 28, there were 68 Ebola cases across seven health zones, exceeding the final case count for the 2018 Equateur Province outbreak. Work also continues to support the DRC Ministry of Health with transition activities following the end of the 2018 eastern DRC Ebola outbreak last month.

A mother with her pups.
Rat-bite fever (RBF) is a rare but serious and potentially fatal disease. A recently published analysis seeks to shed light on the burden of RBF in the United States, estimating the number of RBF hospitalizations, emergency department (ED) visits, and outpatient clinic visits using multiple data sources. The majority of RBF ED visits and hospitalizations were seen among individuals aged 0–19. However, there appeared to be differences in the socio-economic characteristics and insurance coverage of patients seen for RBF ED visits versus hospitalizations, suggesting socio-economic barriers to care.
Given the rarity of RBF, authors expect that the rates reported are an underestimate of the true burden of disease. Healthcare providers should consider RBF for patients (particularly pediatric patients) with symptoms of fever, nausea, vomiting, joint pain, rash, and septic arthritis; and history of known or suspected exposure to rodents. Enhanced awareness and prompt diagnosis can improve health outcomes for vulnerable pediatric populations with RBF infections. Visit CDC’s rat bite fever website, read the article in Open Forum Infectious Diseases, and tune into the September 2 ZOHU Call to learn more.

CDC collaborated with the Council to Improve Foodborne Outbreak Response (CIFOR) to update CIFOR’s Guidelines for Foodborne Disease Outbreak Response. This streamlined third edition of the guidelines is a comprehensive source of information on foodborne disease investigation and control for local, Nestate, territorial, tribal, and federal health agencies.
The updates address rapid and continuing changes in many aspects of food safety, including laboratory technology, data sharing, improved disease detection methods, increasing centralization of food production, and changing eating habits. You can download the guidelines now. A limited number of free, printed versions will be available this fall.
CDC worked with staff from the Georgia Institute of Technology and the Norwegian Institute of Public Health on a recent publication in The Lancet Planetary Health: Human faeces-associated extended-spectrum β-lactamase-producing Escherichia coli discharge into sanitation systems in 2015 and 2030: a global and regional analysis. The authors estimated the mass of feces containing extended-spectrum beta-lactamase (ESBL)-producing E. coli—a major cause of antibiotic-resistant infections—entering different sanitation systems as a measure of the distribution of feces-associated risks globally. Worldwide, approximately 25% of feces that contain ESBL-producing E. coli enter unimproved sanitation systems (systems that do not safely contain feces) or are released directly into the environment without treatment.
Improving management and treatment of feces within sanitation systems could slow the development and transmission of antibiotic-resistant organisms.
On June 26, the US Public Health Service (PHS) released an updated guideline related to testing solid organ donors and transplant recipients for infection with HIV, hepatitis B virus (HBV), and hepatitis C virus (HCV). This update to the 2013 PHS guideline on the same topic was made to increase the use of available organs and enhance safety measures to protect patients from HIV, HBV, and HCV.
Staff throughout NCEZID continue to provide vital support to the COVID-19 pandemic response, either directly with Incident Management leadership, task forces, and field teams, or indirectly by taking on additional duties to maintain other work activities. Despite marked increases in COVID-19 cases and deaths nationwide during July, CDC’s work is making an important difference with contributions in such areas as surveillance data analytics and reporting, epidemiologic studies, laboratory diagnostics, infection control, community mitigation, public health guidance, support to state and local health departments, global migration/travelers’ health, health communication, policy, emergency response management, and more. Here are just a few recent examples of NCEZID staff in action.
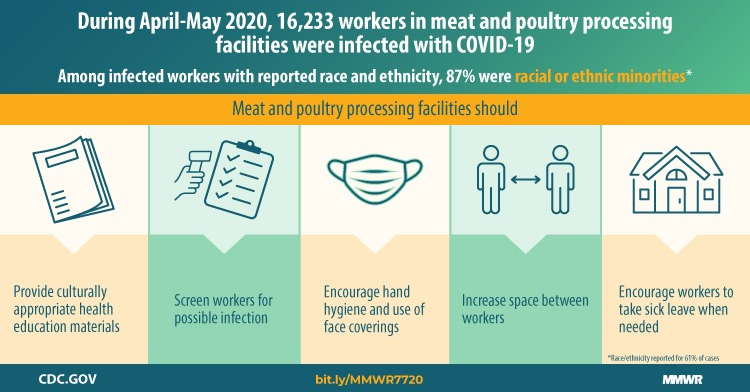
MMWR Update: COVID-19 Among Workers in Meat and Poultry Processing Facilities in the U.S. in April – May
Meat and poultry processing facilities face distinctive challenges in the control of infectious diseases, including coronavirus disease 2019 (COVID-19) (1). COVID-19 outbreaks among meat and poultry processing facility workers can rapidly affect large numbers of persons. Nineteen states reported data on assessments of COVID-19 cases among over 112,000 workers in 115 meat and poultry processing facilities through April 27, 2020, and documented 4,913 cases and 20 deaths (1). This report provides updated aggregate data from states regarding the number of meat and poultry processing facilities affected by COVID-19, the number and demographic characteristics of affected workers, and the number of COVID-19–associated deaths among workers, as well as descriptions of interventions and prevention efforts at these facilities.
Training Activity Team trains over 800 COVID-19 responders
Since the beginning of the COVID-19 response, CDC’s training activity has developed and delivered training sessions to CDC staff (including deployed staff), contractors, and virtual call center agents across multiple CDC centers. The training activity also shares COVID-19 screening updates through their “Bottom Line Up Front” guidance newsletter, which is distributed multiple times a week to CDC staff.
Crisis and Epidemiology Laboratory Capacity (ELC) Cooperative Agreement Team
CDC reviewed 258 work plans for the Crisis and ELC cooperative agreements. In total, the Crisis Response Cooperative Agreement, ELC CARES (Coronavirus Aid, Relief, and Economic Security Act of 2020) funding, and ELC enhancing detection funding provides more than $11.6 billion to state and local health departments for a broad range of COVID-19 prevention and control activities. The CDC team was one of several across the agency providing expert reviews of the cooperative agreement materials.
“On June 25, 42 days after the last survivor tested negative, the Democratic Republic of the Congo (DRC) Ministry of Health and the World Health Organization announced the end of the Ebola outbreak in eastern DRC. The outbreak began in August 2018 and included a cluster of cases in April 2020, ending the first 42-day countdown on day 40. In total, there were 3,470 cases and 2,287 deaths, making the eastern DRC Ebola outbreak the second largest in history. CDC staff played crucial roles in both the Atlanta and field responses to this outbreak. CDC will continue to support capacity building efforts in eastern DRC to ensure quick detection of, and response to, any future cases due to sexual transmission or relapse in a survivor of this outbreak.
Although ending this outbreak is a huge accomplishment, CDC’s Ebola response work in DRC continues. On June 1, a new outbreak of Ebola was confirmed in Equateur Province, the same area of DRC that experienced the outbreak in early 2018. Sequencing confirmed that the outbreak is due to a new introduction of the virus and not linked to the 2018 outbreaks in Equateur Province or eastern DRC.”
CDC scientists have developed a model that uses viral RNA concentrations in sewage to predict the overall prevalence of SARS-CoV-2 infection in a community served by a sewer system. They aim to find out if sewage may be an early warning for the presence of SARS-CoV-2, the virus that causes COVID-19. The team is now collaborating with the Environmental Protection Agency, the University of South Carolina, Stanford University, Hampton Roads Sanitation District in Virginia, and other partners to assess the model using sewage data collected from several U.S. locations.

CDC released a new MMWR: “Update on Extensively Drug-Resistant Salmonella Serotype Typhi Infections Among Travelers to or from Pakistan and Report of Ceftriaxone-Resistant Salmonella Serotype Typhi Infections Among Travelers to Iraq—United States, 2018–2019.” The report highlights findings from CDC’s enhanced surveillance system showing that some Salmonella Typhi bacterial infections linked to travel to Pakistan and Iraq are resistant to ceftriaxone, an antibiotic used to treat typhoid fever. The emergence of ceftriaxone-resistant infections underscores the importance of pre-travel vaccination and safe food and water practices. CDC also created new fact sheets and posters for travelers and healthcare professionals, which are available in Bengali, English, Hindi, and Urdu.
NCEZID divisions, leadership, and staff are an integral part of CDC’s and the federal government’s response to the ongoing COVID-19 pandemic. Here are just a few examples of NCEZID’s work in the fight against COVID-19:
ELC awards $10.25 billion to 64 jurisdictions across the United States
On May 18, awards totaling $10.25 billion were provided to the 64 recipients of the Epidemiology and Laboratory Capacity (ELC) for Prevention and Control of Emerging Infectious Diseases (ELC) Cooperative Agreement. Funding was made possible from the Paycheck Protection Program and Health Care Enhancement Act (PPPHEA) and constitutes the largest funding opportunity any one CDC program has ever dispersed. This financial support, called ELC Enhancing Detection, is to help states, localities, and territories develop, purchase, administer, process, and analyze COVID-19 tests, and conduct surveillance, contact tracing, and related activities. ELC Enhancing Detection awards will complement, not duplicate, existing funding provided to jurisdictions, including the ELC Community-based Surveillance and ELC CARES supplements. A detailed breakdown of all COVID-19 funding, by jurisdiction, can be found online [PDF – 1 page].
CDC launches national viral genomics consortium to map the transmission of SARS-CoV-2
CDC has kicked off the SARS-CoV-2 Sequencing for Public Health Emergency Response, Epidemiology, and Surveillance (SPHERES) consortium, which will greatly expand the use of whole genome sequencing (WGS) of the COVID-19 virus.
SPHERES is an ambitious effort to coordinate SARS-CoV-2 genome sequencing nationally, organizing dozens of smaller efforts into a network of laboratories, institutions, and corporations. The consortium combines the expertise, technology, and resources of 37 state and local public health departments, several large clinical laboratories, and over two dozen collaborating institutions across the federal government, academia, and the private sector. SPHERES will accelerate open data sharing and establish best practices, consensus data standards, and a pool of resources and expertise to bring cutting-edge technology to the national COVID-19 response.
SPHERES will provide real-time sequence data to public health response teams investigating cases and clusters of COVID-19 across the country. It will help them better understand how the virus is spreading. And better data will help public health officials protect and save lives.

CDC’s Foodborne Diseases Active Surveillance Network (FoodNet) released a new report showing that progress has stalled in controlling foodborne pathogens in the United States. Recent increases in foodborne illness might be due in part to increased testing and improved technologies, such as culture-independent diagnostic tests and whole genome sequencing, that have revealed infections which might not have been diagnosed in the past. More resources are needed to reach the full potential of these technologies, and targeted approaches to prevention are needed to reduce foodborne illness.

CDC’s Rickettsial Zoonoses Branch published the Guide to the Surveillance of Metastriate Ticks (Acari: Ixodidae) and Their Pathogens in the United States [PDF – 55 pages]. The guidance is intended to provide recommendations for the collection and processing of ticks for tick and tickborne pathogen surveillance efforts.

Each year, Healthy and Safe Swimming Week focuses on simple steps everyone can take to help ensure healthy and safe swimming experiences. This year’s theme, “Stay Safe and Healthy in Your Backyard Pool,” aimed to educate backyard pool owners on steps they can take to keep themselves and others in their household free of injury and illness. DFWED raised awareness through a feature for the public, a communications toolkit for partners, and other materials.
NCEZID divisions, leadership, and staff are an integral part of CDC’s and the federal government’s response to the ongoing COVID-19 pandemic. Here are just a few examples of NCEZID’s work in the fight against COVID-19:
ELC awards record $631 million to 64 jurisdictions across the United States
In April 2020, CDC awarded $631 million to 64 jurisdictions across the United States through the Epidemiology and Laboratory Capacity for Prevention and Control of Emerging Infectious Diseases (ELC) cooperative agreement. These awards are the largest the ELC program has ever dispersed. The funds come from the Coronavirus Aid, Relief, and Economic Security (CARES) Act of 2020 and are designed to help jurisdictions improve their ability to identify COVID-19 cases, conduct contract tracing and follow-up, and implement containment measures. The funds also enable jurisdictions to improve morbidity and mortality surveillance, enhance testing capacity, control COVID-19 in high-risk settings and protect high-risk populations, and work with healthcare systems to manage and monitor system capacity of their surveillance systems.
NCEZID’s Division of Healthcare Quality Promotion (DHQP) expertise supports CDC COVID-related surveillance
The Division of Healthcare Quality Promotion (DHQP) programs helped to establish a pathway for healthcare facilities to report COVID-19 data to the National Healthcare Safety Network (NHSN) surveillance system. Acute-care hospitals and long-term care facilities can now use NHSN to report COVID-19 patients and other crucial information to CDC and state and local health departments. Efforts to expand this capacity in a tailored way to other healthcare settings (e.g., dialysis) are being explored. A new Centers for Medicare & Medicaid Services rule will require nursing homes to report cases to CDC.
Control and prevent further spread of COVID-19 on cruise ships and in communities
The Division of Global Migration and Quarantine (DGMQ), along with staff detailed to the Cruise Ship Task Force (CSTF) that was temporarily active as part of CDC’s COVID-19 response, worked tirelessly to control COVID-19 on cruise ships and prevent further spread of COVID-19 into communities. Teaming up with the US Coast Guard, CDC staff tracked about 100 vessels, oversaw the safe disembarkation and repatriation of more than 260,000 cruise ship passengers and crew members, and provided support for triage and medical evacuations to 41 cruise ships affected by COVID-19. In March, CDC issued the first ever industry-wide No Sail Order to prevent all new passenger embarkations. This order was extended in April as cruise lines develop and implement plans to provide a safe work environment for crew members. DGMQ continues to help crew members return home safely during this period of suspended operations.

CDC, with state and federal partners, is investigating several multistate enteric disease outbreaks, including Listeria infections linked to enoki mushrooms imported from Korea. Thirty-six people from 17 states have become sick. Three companies have recalled the mushrooms and a firm in Korea has been put on import alert.

CDC scientists have been interviewed about the safe handling of backyard flocks after recent media articles reported an increase in people keeping backyard flocks for fresh eggs because of COVID-19. Read more about safely handling backyard flocks and preventing Salmonella.

Gouthami Rao (DFWED) and Kaunda Williams (VIDOH) oversee the collection of a water sample from a household cistern to test for evidence of waterborne pathogens.
CDC led a large-scale cistern water evaluation in the US Virgin Islands, in partnership with the US Virgin Islands Department of Health (VIDOH) and Love City Strong, a local nongovernmental organization. Following the 2017 hurricane season, VIDOH identified the need for evidence-based recommendations for making household cistern water safe for consumption during and after emergencies. More than 90% of the population relies on cisterns as their main residential water supply. The team administered a survey and tested the cistern and tap water of 400 households for E. coli. A smaller number of households received additional testing for other pathogens. The evaluation found that 80% of water taken directly from the cistern hatch tested positive for E. coli contamination, and 58% of cistern water taken from a kitchen tap also tested positive. The team is working to identify and communicate environmental and household management practices to help residents address specific contamination risks for their cisterns.
DHCPP's Amanda MaCgurn (L) discusses response data with CGH surveillance deployer Charlene Siza in Goma, DRC.
CDC is a year and a half into the second-largest Ebola outbreak on record. Weekly case counts in Democratic Republic of Congo (DRC) have been in the single digits for most of the year to date. Late this month, there was an entire week without a case for the first time since the outbreak began.
However, there needs to be six straight weeks with no new cases—a total of 42 days in a row—plus 90 days of enhanced surveillance to be able to call this outbreak over. The World Health Organization (WHO) recently reaffirmed the outbreak’s status as a Public Health Emergency of International Concern, warning that the security situation in the region leaves open the potential for new cases. WHO says it will revisit that decision within two months. In the meantime, CDC responders will keep working in Atlanta and with the DRC and its neighbors to support the response and preparedness efforts until the outbreak can definitively be declared over.
In January, the Making Dialysis Safer for Patients Coalition and the American Association of Kidney Patients released a video for dialysis staff and patients on dialysis about the importance of speaking up to prevent infections and improve patient safety. The video follows the journey of two patients on dialysis who feel empowered to speak up and share concerns about their treatment. The video also highlights ways dialysis staff can create an environment where patients feel safe speaking up. Along with the video, the group created a handout for staff with helpful tips and reminders about how to engage patients and caregivers. The video was released ahead of Patient Safety Awareness Week, which CDC observes from March 8-14.

Researchers remove bats that are caught in nets.
CDC scientists and partners (including University of California-Davis and Sierra Leone’s Njala University and University of Makeni) have discovered active circulation of an Angola-like strain of Marburg virus in Egyptian rousette fruit bat colonies for the first time in Sierra Leone. Actively infected bats can potentially spread the virus to people who are in close contact with them, including when people prepare or eat fruit that’s been contaminated with the saliva, feces, or urine of an infected bat. Unfortunately, the bats eat a lot of the same fruit that we do. CDC has worked closely with partners in Sierra Leone to educate residents about conserving this ecologically beneficial bat species and the importance of avoiding the bats and their caves to prevent the spread of Marburg virus to people. Read more in the January 24 issue of Nature.
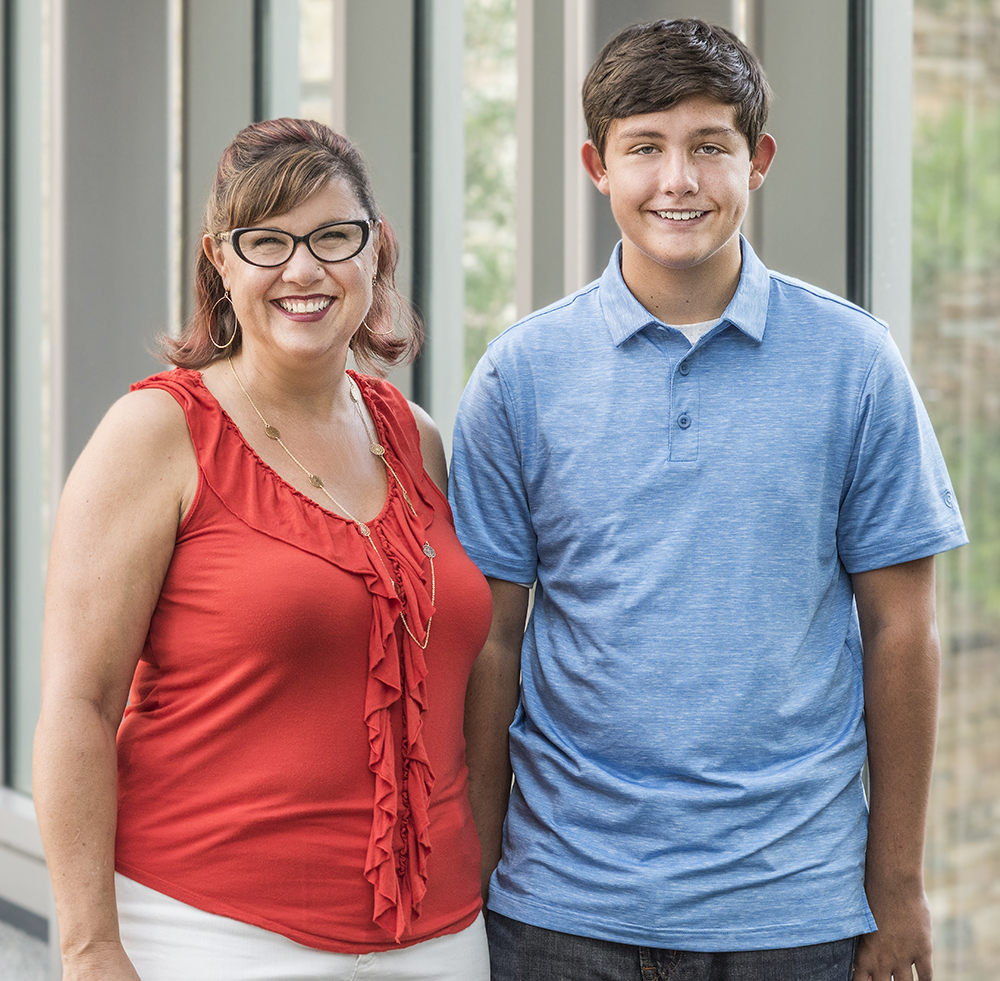
CDC’s new video series, “Was It Something I Ate?,” presents stories of people who developed serious intestinal infections from food or animal contact. The stories are from families with children who developed Salmonella infection from eating contaminated chicken or contact with backyard poultry, and from a CDC veterinarian who investigated an outbreak linked to working with farm animals.
These stories highlight the importance of preventing infections from food or animal contact through efforts by industry, government, and the public. Check out all videos in the series (as well as free graphics, Medscape commentaries, and more) in the Resource Library section of CDC’s food safety website.

Nearly 400 representatives from across the country attended CDC’s first Vector Week, held March 25-28. CDC’s Division of Vector-Borne Diseases Director, Lyle Petersen, presented a collective vision and strategy to battle vector-borne diseases nationally. Other CDC senior scientists and experts from state and local public health programs and the Centers of Excellence presented on specific challenges and opportunities for vector-borne disease prevention and control. CDC and other public health programs are at a crucial juncture in our efforts to prevent and control vector-borne diseases, and we hope the deliberations at Vector Week 2020 will shape new directions in this important area.

(L) NASA's Alvin Smith, Michael Calaway, Michael Myer, Richard Mattingly, and Andrea Harrington
CDC has been consulting with the National Aeronautics and Space Administration (NASA) on safety issues surrounding the Mars Sample Return mission. The proposed mission will use rovers to sample Martian soil and bring back specimens to Earth for testing. A NASA team visited CDC earlier this month to discuss how to make sure that any pathogens that might be in the samples don’t pose a risk to people, agriculture, or the environment.
NASA staff also met with staff here at CDC about security and engineering of high-containment labs and biosafety for working with the samples. We talked about how to either contain or sterilize samples to prevent contaminants from getting in or out. Last week, representatives from CDC traveled to Salt Lake City, Utah, to meet with NASA’s Sterilization Workgroup, where they explained how CDC communicates about infectious disease risks and outbreaks. CDC shared examples of ways we have communicated about high-consequence but low-probability diseases.
On February 5, NCEZID released its 2019 Accomplishments highlighting everything from protecting domestic and global public health threats to collaborating with our partners to make an even bigger mark in saving lives and strengthening our preparedness to fight emerging and zoonotic infectious diseases. You can view NCEZID’s 2019 Accomplishments through a PDF – 16 pages or on our website.
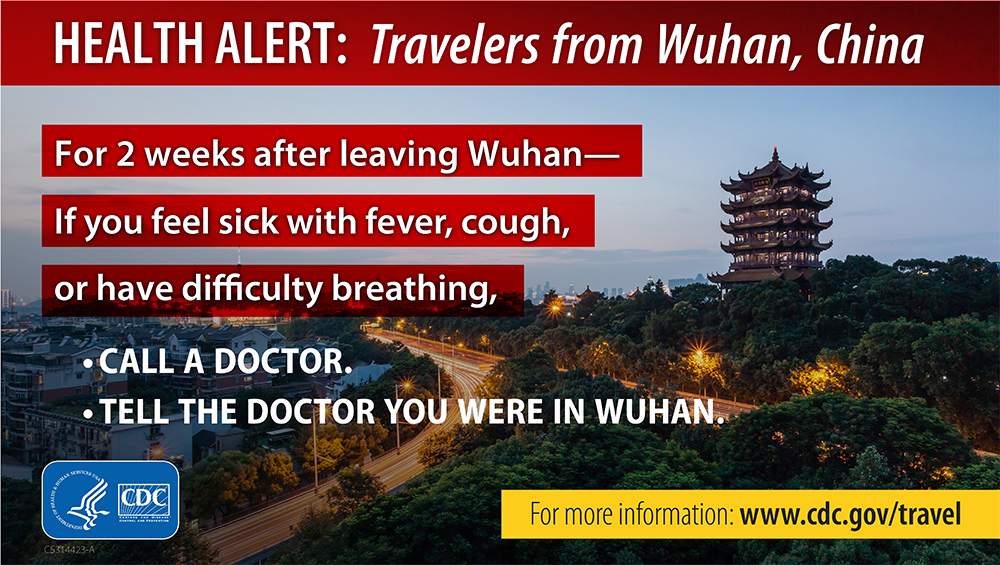
Since early January, CDC has been actively engaged in the international response to the rapidly escalating outbreak of respiratory infections linked to the 2019 novel coronavirus (2019-nCoV). CDC has activated its Emergency Operations Center under the leadership of National Center for Immunization and Respiratory Diseases (NCIRD), with support from NCEZID and other centers across the agency. Information about the outbreak has been changing daily. CDC and its public health partners have launched an aggressive preparedness and response effort. NCEZID’s response activities cut across programs throughout the center, as these examples show:
- Conducting enhanced health screenings at US airports, travel health notices, travel health alert messages in airports, and other travel- and quarantine-related activities, including analysis of travel data.
- Sharing infection control guidance.
- Providing expertise for pathology studies.
- Supporting efforts to develop and distribute laboratory diagnostic kits.
- Providing leadership and support for field deployments and CDC’s Emergency Operations Center.

On December 28, Puerto Rico experienced the first of a series of earthquakes. On January 7, the island suffered a 6.4 magnitude earthquake. A 5.9 magnitude aftershock followed on January 11, and more than 2,300 tremors have occurred since December 28. We are communicating regularly with our staff in Puerto Rico to ensure that they are safe, and Dengue Branch facilities in San Juan have not been damaged. Metro areas currently have power, but southern Puerto Rico is still experiencing outages. Several CDC staff are participating in efforts to aid residents in this part of the island. CDC is actively engaged and monitoring quake activity and are on standby to provide support if needed.

People walking in Mpondwe, Uganda, near the country's border with the Democratic Republic of the Congo.
Case counts have fallen from more than 100 a week at the worst of the outbreak to the single digits for many weeks. But the remaining hot spots are in places where surveillance and contact tracing are difficult, and recent violence has disrupted response work by some of our partner agencies.
Ebola vaccine receives FDA approval
In December, the US Food and Drug Administration (FDA) approved Ervebo, Merck’s Ebola vaccine, for use in the United States in people 18 and older. It’s the first FDA approval of a vaccine for Ebola virus, marking a historic milestone. The Democratic Republic of the Congo Ethics Review Committee and National Regulatory Authority have approved the Merck rVSV-ZEBOV vaccine in the DRC for this outbreak under “expanded access.” The existing vaccine supply in DRC and neighboring countries will remain investigational. This vaccine has been shown to be safe and protective against the Zaire ebolavirus species.

CDC, with state and federal partners, is investigating several multistate enteric disease outbreaks, including the following:
- Listeria infections linked to hard-boiled eggs produced by Almark Foods of Gainesville, Georgia. One death in Texas has been reported among seven total illnesses. On December 23, Almark Foods recalled all hard-boiled eggs produced at the Gainesville facility.
- Multidrug-resistant Campylobacter infections linked to contact with puppies in pet stores. Whole genome sequencing shows that the strain causing illness in 2019 is closely related genetically to the strain that caused a similar outbreak in 2016–2018.
- Salmonella infections linked to cut fruit. People in 11 states have gotten sick from eating contaminated cut honeydew melon, cantaloupe, or pineapple produced by Tailor Cut Produce.
- Salmonella infections linked to small pet turtles. People in 9 states have been infected with Salmonella typhimurim likely from contact with small pet turtles. The U.S. Food and Drug Administration bans the sale and distribution of turtles with shells less than 4 inches long as pets, but these animals can still be found for sale at flea markets, swap meets, and online.
Medical illustration of mehicillin-resistant Staphylococcus aureus (MRSA) bacteria, as pictured in the AR Threats Report
CDC released a new interactive case assessment tool on Medscape to help healthcare providers learn more about preventing deadly Staphylococcus aureus (staph) infections in their patients. The tool was released in connection with a 2019 issue of Vital Signs that reported that 119,000 people suffered from bloodstream staph infections in the United States in 2017—and nearly 20,000 died. CDC called on healthcare facilities, providers, and administrators to protect patients from device- and procedure-related staph infections and promoted tools and resources to support those efforts. This case assessment tool is the latest resource created to help providers protect their patients against serious staph infections that can lead to sepsis or death.

CDC’s Arctic Investigations Program (AIP) recently published an article in Gastroenterology that summarizes the outcomes of a meeting that brought together international gastric cancer experts, Alaskan health providers, Alaska Native community and tribal leaders, public health officials, and representatives from other North American indigenous populations. The article describes the need for solutions designed to work in Alaska, where approximately 40% of Alaska Native people live in communities not connected to a road system. Participants identified the need for targeted screening and surveillance, clinical and community education, and additional research to uncover why gastric cancer rates are disproportionately high among Alaska Native people. AIP and its partners in Alaska have begun to address these needs, including designing a long-term screening study.