Our Work: 2018
Our Work - 2018
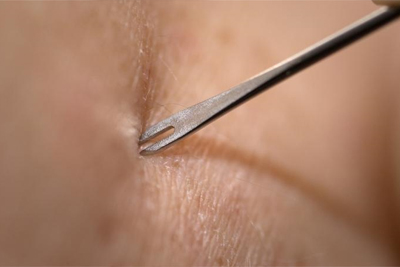
CDC is providing clinicians, laboratory scientists, public health professionals, and the public the information they need to prepare for and respond to a smallpox emergency. NCEZID staff recently released a series of videos that instruct clinicians how to administer smallpox vaccine by using the bifurcated needle, interpret vaccination results, care for the vaccination site, and manage common reactions and potential serious adverse events. The videos provide a way to educate clinicians and vaccine administrators quickly, should a smallpox emergency ever occur.
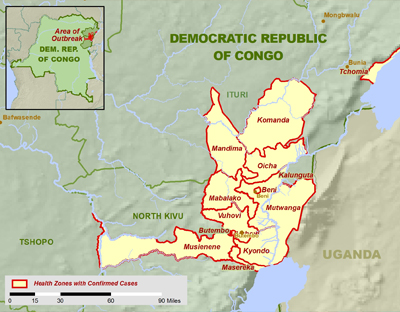
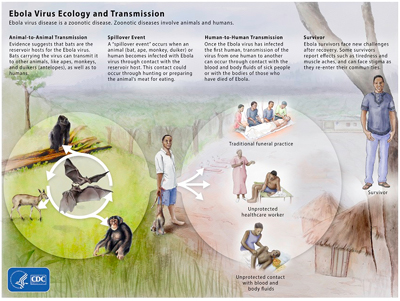
The Ebola outbreak in eastern Democratic Republic of the Congo (DRC) continues unabated nearly four months after it was announced on August 1. It’s the 10th outbreak in DRC since the discovery of Ebola in 1976. As of November 24, 412 confirmed and probable cases, including 236 deaths, had been reported, making this the single largest Ebola outbreak in DRC’s history. Significant challenges continue to thwart the response. Despite having deployed about 90 staff to work on the response since the outbreak began, CDC has been limited in its ability to support on-the-ground efforts in the outbreak’s epicenter because of ongoing security risks. The armed conflict in the area is the most prominent challenge, keeping some responders out and limiting effective contact tracing and other activities necessary to contain the outbreak
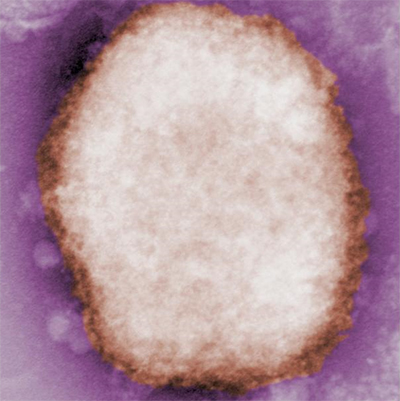
New cases continue to be detected in Nigeria’s monkeypox outbreak, which began in September 2017; as of November 2018, the country reports a total of 300 cases (126 confirmed), including seven deaths. CDC staff have supported the Nigeria Centre for Disease Control by providing onsite trainings for medical, public health, animal health, and laboratory officials; technical consultation on suspected cases; monkeypox-specific tools for investigations; expertise in database management; and quality control of diagnostic assays at the national public health laboratory. From Atlanta, staff have also confirmed test results obtained in Nigeria and performed genetic sequencing to learn more about how the monkeypox virus strains are related.
Also worrisome are recent travel-related monkeypox cases that are linked to the Nigerian outbreak. In the United Kingdom, three such cases were reported in September, including two unrelated cases in travelers to Nigeria and a third case in a healthcare worker. Israel reported an imported case in October. In response, CDC posted a Level 2 Alert Travel Notice for monkeypox in Nigeria in mid-October.
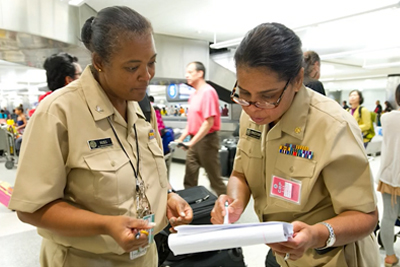
To celebrate the 50th anniversary of the quarantine program at CDC, NCEZID’s Division of Global Migration and Quarantine developed a short video that chronicles CDC’s quarantine legacy.
Quarantine came out of the Venetian practice that began in the 1300s to protect against importing bubonic plague. American quarantine law goes back to the colonies in 1647 and has served as the cornerstone of public health. In 1798, President John Adams and Congress created the US Marine Hospital Service, which established a network of hospitals and staff along the coast to protect against the spread of disease. This network became the US Public Health Service.
Today, CDC has 20 quarantine stations strategically located at US airports, land borders, and seaports where most international travelers arrive. DGMQ is responsible for upholding US quarantine regulations to protect our country’s borders from contagious diseases. Check out the video for more information about the fascinating history of the US quarantine program.

Foodborne disease outbreaks received national attention in November. CDC is investigating several new and ongoing outbreaks across the country, including:
- Salmonella infections linked to tahini from Achdut Ltd.
- Listeria infections linked to pork products produced by Long Phung Food Products
- E. coli infections linked to romaine lettuce
- Salmonella infections and recalled Duncan Hines cake mix
- Multidrug-resistant Salmonella infections linked to raw chicken products
- Salmonella infections linked to ground beef
- Multidrug-resistant Salmonella infections linked to raw turkey products
- Salmonella infections linked to kosher chicken
A new surveillance summary provides information on 839 foodborne disease outbreaks reported to CDC in 2016. These outbreaks resulted in 14,259 illnesses, 875 hospitalizations, 17 deaths, and 18 food product recalls. Norovirus (145 outbreaks) and Salmonella (132 outbreaks) were the most commonly reported causes. The most common food categories linked to outbreaks were fish (26 outbreaks), mollusks (such as oysters and scallops, 21), dairy (19), and pork (18). The food categories responsible for the most outbreak-associated illnesses were mollusks (529 illnesses), pork (438), grains and beans (383), and chicken (356). Restaurants were the most commonly reported location where food was prepared (459 outbreaks), specifically restaurants with sit-down dining (363).
The data come from reports that state, local, and territorial public health agencies submitted to the Foodborne Disease Outbreak Surveillance System through the National Outbreak Reporting System (NORS), and includes single-state and multistate outbreaks.

CDC is investigating several outbreaks linked to food products:
- A multistate outbreak of multidrug-resistant Salmonella Infantis infections has resulted in 92 cases reported from 29 states. Evidence suggests that many types of raw chicken products from a variety of sources are a likely source of this outbreak. Consumers and retailers should always handle raw chicken carefully and cook it thoroughly to prevent illness.
- CDC and USDA are investigating a multistate outbreak of Salmonella Newport infections linked to ground beef produced by JBS Tolleson, Inc., of Tolleson, Arizona. The company recalled approximately 6.5 million pounds of beef products that may be contaminated. As of October 23, 120 cases had been reported.
- A multistate outbreak of Listeria infections was linked to ready-to-eat deli ham produced by Johnston County Hams, Inc., in Smithfield, North Carolina. Several companies have recalled the ham products, and people should not eat, sell, or serve these recalled ready-to-eat ham products.
CDC recently published the 2016 Healthcare-Associated Infections Progress Report, which shows year-to-year progress on the prevention of key healthcare-associated infections (HAIs) to highlight progress and target areas for improvement.
The report shows that overall, prevention progress has been made, but more work is needed. Specifically, acute care hospitals saw significant reductions in most HAIs across the board, with the exception of some types of surgical site infections. Greatest prevention improvements were seen for central line-associated bloodstream infections, particularly in neonatal intensive care units.
The 2016 HAI Progress Report is the first report to measure year-to-year HAI prevention progress against the 2015 baseline and is the first progress report to be published in the AR Patient Safety Atlas. Moving forward, CDC will publish progress report data in the Atlas to make the data more accessible and easier to view.

CDC’s Travelers’ Health launched the Think Travel campaign for healthcare providers to build greater awareness of the need to incorporate travel health into patient care. The campaign includes resources to help providers talk with patients before and after their trips about health risks and possible exposures related to travel.
Dr. Casey Barton Behravesh, a veterinarian and Director of the CDC One Health Office, appeared on an episode of The Dr. Oz Show to discuss recent reports of Capnocytophaga infections in people linked to dogs. On the show, Dr. Barton Behravesh explained the facts about this rare disease, while also providing tips on how to stay healthy while enjoying your dogs and other pets.

During the United Nations (UN) General Assembly on September 25, the United States launched the AMR Challenge, a yearlong effort spearheaded by HHS and CDC to call global stakeholders to action on antimicrobial resistance (AMR). During the kick-off, participants described the global threat of AMR and its impact on all people and industries, underscored how everyone can slow its development and spread, and highlighted success stories. The event included organizations that had already made commitments or submitted a commitment in at least one of five action categories: infection prevention and control; antibiotic use; vaccine, therapeutic, and diagnostic development; environment and sanitation; and tracking and data. To date, there have been 99 commitments from over 100 partner organizations and countries.
September was Sepsis Awareness Month, and marked the 1-year anniversary of the launch of Get Ahead of Sepsis, CDC’s national educational effort that promotes early recognition and timely treatment of sepsis, as well as the prevention of infections that could lead to sepsis. Each year, at least 1.7 million Americans develop sepsis, and nearly 270,000 die as a result. As part of outreach efforts, CDC launched this public service announcement.

As of September 6, 2018, three US cases of leptospirosis were identified among travelers who had visited Israel, with additional suspected cases reported and under investigation. Meanwhile, dozens of cases have been confirmed in Israel by the Ministry of Health, and hundreds more people have reported symptoms. The outbreak has affected people who had been exposed to seven natural water sources in the Golan Heights region of northern Israel. In response, CDC quickly developed and posted a Health Alert Network (HAN) advisory alerting clinicians to the travel-associated risks and advising them about appropriate diagnosis and treatment methods. CDC also posted a Watch Level 1 Travel Notice.

Check out two new “I Am CDC” videos that spotlight NCEZID employees and their work. Amanda MacGurn highlights her time with CDC’s Global Border Health Team, where she works with authorities in international airports and other points of entry in French-speaking West African countries to help them plan for infectious disease outbreaks. And CDC entomologist Janet McAllister discusses her work as a research entomologist in Fort Collins, CO, and remembers helping Miami-area communities control mosquitoes during the Zika outbreak there.
Only one week after the Ebola outbreak in western Democratic Republic of Congo (DRC) was declared over on July 24, an unrelated cluster of Ebola cases was reported about 800 miles away in Nord-Kivu Province in the eastern part of the country, along the border with Uganda. Since then, the outbreak has spread and sickened more people. CDC is working closely with the DRC Ministry of Health, the World Health Organization, and other international partners. CDC has deployed Ebola experts from its Viral Special Pathogens Branch to provide on-the-ground assistance in Beni, near the outbreak’s epicenter. Additional staff have contributed to outbreak management from WHO in Geneva and provided lab training and assistance to Rwandan health officials. Additionally, CDC is assisting with border health, risk communications, community engagement, emergency response management, and other areas. The remote location of the outbreak’s epicenter, combined with security concerns, are challenges responders are working to overcome. See CDC’s Ebola website for additional information.

August 20-24 marked the fifth annual Contact Lens Health Week, organized by CDC in close collaboration with partners as a strategy to increase public awareness and promote healthy contact lens wear and care.
While contact lenses are usually a safe and effective form of vision correction, they are not entirely risk-free – especially if they are not cared for properly. Learn more about taking care of contact lenses and read a new MMWR article describing a case series of people who developed eye infections linked to sleeping in lenses.

CDC held its 10th occurrence of the International Conference on Emerging Infectious Diseases (ICEID) from August 26-29 in Atlanta, GA. Held every 2-3 years, the conference brought together more than 1,500 public health professionals from around the world to encourage the exchange of the latest information on issues affecting the emergence, spread, and control of infectious diseases. Major topics for ICEID 2018 included surveillance and outbreak response, laboratory diagnostics and systems, factors affecting disease emergence and control, and public health preparedness.

Rocky Mountain spotted fever (RMSF) is the most deadly tickborne disease in the United States. Each year, 3,000-5,000 cases of RMSF and other spotted fever rickettsioses are reported in the US, including 5-10 deaths and substantially more severe cases. Effective treatment is available, and severe and fatal cases of RMSF can be prevented through early recognition and treatment. CDC has a new toolkit for healthcare providers, epidemiologists, and public health practitioners to aid in the diagnosis and treatment of RMSF and other tickborne diseases. The toolkit includes free Continuing Education in seven professional categories: CME, CNE, CEU, CECH, AAVSB/RACE, CPE, and CPH.

CDC has released the 2018 edition of the Model Aquatic Health Code (MAHC). Government officials and the aquatics sector can use the MAHC to create or update existing pool codes and reduce risk of outbreaks, drowning, and pool-chemical injuries. Learn how the MAHC helps make swimming and other water activities healthier and safer.
CDC is investigating several outbreaks linked to food products.
- A multistate outbreak of multidrug-resistant Salmonella Reading infections has been linked to raw turkey products in 26 states, resulting in 90 cases of illnesses of July 11. Raw turkey should always be handled carefully and cooked thoroughly.
- A Food Safety Alert was issued for a multistate outbreak of Salmonella Sandiego linked to Spring Pasta Salad at Hy-Vee grocery stores in five states, with 21 people infected as of July 1. Consumers should not eat recalled Hy-Vee Spring Pasta Salad.
- A multistate outbreak of Vibrio parahaemolyticus infections has been linked to fresh crab meat imported from Venezuela. Twelve people in three states and the District of Columbia have been reported to be infected after eating fresh crab meat from Venezuela. Consumers should not eat, restaurants should not serve, and retailers should not sell fresh crab meat imported from Venezuela at this time.
- CDC continues to investigate a multistate outbreak of Salmonella Mbandaka infections linked to Kellogg’s Honey Smacks Cereal. As of July 12, 100 people had been infected in 33 states. CDC continues to recommend that consumers not eat any Kellogg’s Honey Smacks cereal.

A new CDC Museum exhibit, The Refugee Journey to Wellbeing, provides insight into refugee health and the resettlement process. The exhibit introduces visitors to the programs and processes supporting refugee health along the journey from displacement to resettlement in the United States. Its installation at the David J. Sencer CDC Museum is the first public showing of this hands-on exhibit, created in 2016 by CDC’s Division of Global Migration and Quarantine, and the Emergency Response and Recovery Branch, Division of Global Health Protection, in partnership with the American Society of Tropical Medicine and Hygiene. The exhibit will be on display from July 9-October 5, 2018.
CDC is working with state and federal partners to investigate several multistate outbreaks, including the following:

- Salmonella infections linked to live poultry in backyard flocks. As of June 1, 124 sick people have been reported from 36 states; 31% of those people are children younger than 5 years old. Since 2000, 70 outbreaks of Salmonella infections have been linked to contact with backyard flocks.
- Salmonella infections linked to pre-cut watermelon, honeydew, cantaloupe, and fruit salad mixes with melon. Of the 70 ill people reported as of June 19, most are older than 60; 34 people have been hospitalized. On June 8, Caito Foods recalled pre-cut melon products that were sold in many different stores in Georgia, Illinois, Indiana, Kentucky, Michigan, Missouri, North Carolina, and Ohio. A list of the recalled products is posted on FDA’s website.
- Salmonella infections linked to Kellogg’s Honey Smacks Cereal (see our tweet, retweeted by HHS Secretary Alex Azar, above). As of June 15, the outbreak had sickened 73 people in 31 states. On June 14, the Kellogg Company recalled Kellogg’s Honey Smacks cereal. People should not eat Kellogg’s Honey Smacks cereal, and retailers should not sell or serve recalled cereal.

CDC sent staff to help local health officials investigate and control several anthrax outbreaks in Uganda. To date, there have been more than 150 probable human cases and more than 700 livestock deaths. While in the field, they investigated cases in animals and humans, collected specimens, and provided recommendations for postexposure prophylaxis and guidance on surveillance and anthrax control among livestock. They also helped local lab officials set up training and testing at non-traditional sites like an agricultural institute and regional vet lab. Confirmatory testing is under way in Uganda. Though the team has returned to Atlanta, CDC continues to work closely with Uganda on the ongoing outbreaks.
NCEZID staff from the Division of High Consequence Pathogens and Pathology were featured in a video by WIRED, in which they demonstrated donning personal protective equipment (PPE), told war stories about getting infested with fly larva, and talked about missing family and how hot and uncomfortable our work abroad can be. The WIRED video series “What’s In Your Bag?” highlights the special equipment that various professionals take when they travel. The 17-minute recording is available on YouTube and WIRED’s site.
CDC released an updated reference manual for healthcare providers on tickborne diseases of the United States. Tickborne diseases are becoming more common, and from May through July, people will get more tick bites and tickborne diseases than any other time of year in the United States. Healthcare providers should be aware of the risks for tickborne diseases as well as ways to prevent, diagnosis, and treat them.
The manual provides information to help clinicians:
- Recognize the signs of tickborne disease,
- Understand diagnostic tests and lab findings, and
- Quickly find treatment recommendations

CDC is working closely with the Ministry of Public Health of the Democratic Republic of Congo (DRC), the World Health Organization (WHO), and other partners to investigate an outbreak of Ebola virus disease in the northwestern part of the country. A CDC Ebola Coordination Team in Atlanta is managing the agency’s efforts to support the response in several areas, including epidemiology, laboratory diagnostics, infection prevention and control, border protection, emergency operations, risk communication, and vaccination strategy. As of June 6, WHO had reported a total of 60 Ebola cases (37 confirmed, 14 probable, and 9 suspected), including 27 deaths, since early April. Reports of several confirmed cases in Mbandaka (population 1.5 million) along the Congo River have raised concerns about the risk of disease spreading within DRC and to neighboring countries. On May 18, a WHO emergency committee assessed the situation in DRC and determined that current conditions do not support declaring a Public Health Emergency of International Concern. Learn more about the outbreak.

A new rabies test developed by CDC and partner organizations could result in people who’ve been exposed to potentially rabid animals foregoing the weeks-long regimen of shots needed to prevent the deadly disease. The new LN34 test, designed for use in animals, can more easily and precisely diagnose rabies infection, according to a study recently published in PLOS One. During the pilot study, the test produced no false negatives, fewer false positives, and fewer inconclusive results. It could allow doctors and patients to make better informed decisions about who needs treatment for rabies.
“Many of the areas hardest hit by rabies are also the areas least prepared to run current tests to diagnose it,” said Crystal Gigante, the study’s first author. “The LN34 test has the potential to really change the playing field. Quickly knowing who needs to receive rabies treatment—and who does not—will save lives and families’ livelihoods.”

Many Alaskans have a close relationship with their environment, which often puts them into contact with wild animals—and potentially zoonotic infectious agents. Researchers in DPEI’s Arctic Investigations Program have been studying how some groups of Alaskans might be exposed to certain infectious agents, specifically the diarrheal-disease causing Giardia duodenalis and Cryptosporidium species. They recently published a study that identifies the seroprevalence for these two intestinal protozoa among wildlife biologists, sport hunters, and subsistence hunters and their families. The study showed increased exposure to Giardia among persons living in communities with less access to in-home running water and sanitation services. The study’s findings establish a baseline for exposure to two important infectious organisms that are likely to be affected by changes in the environment; this is an important resource to evaluate changes over time.
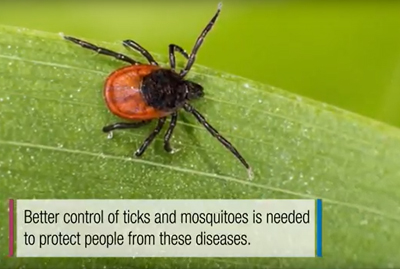
Almost everyone has been bitten by a mosquito, tick, or flea. These can be vectors for spreading pathogens (germs). A person who gets bitten by a vector and gets sick has a vector-borne disease, like dengue, Zika, Lyme, or plague. Between 2004 and 2016, more than 640,000 cases of these diseases were reported, and 9 new germs spread by bites from infected mosquitoes and ticks were discovered or introduced in the US. State and local health departments and vector control organizations are the nation’s main defense against this increasing threat. Yet, 84% of local vector control organizations lack at least 1 of 5 core vector control competencies. Better control of mosquitoes and ticks is needed to protect people from these costly and deadly diseases. Learn more in the May issue of Vital Signs.

CDC is working with several state and federal partners to investigate a multistate outbreak of Escherichia coli O157:H7 infections linked to romaine lettuce from the Yuma, Arizona growing region. Within eight days of first detecting the outbreak in PulseNet, CDC and its partners warned US consumers to throw away all store-bought chopped romaine lettuce at home, including salads and salad mixes containing chopped romaine. Restaurants and retailers were told not to serve or sell any chopped romaine from the Yuma, Arizona growing region. As the team learned more, the warning was expanded to include all romaine lettuce, including whole heads and hearts of romaine lettuce. No deaths have been reported. This outbreak investigation is ongoing.

CDC and partners also are investigating a multistate outbreak of Salmonella Braenderup infections linked to shell eggs. As of April 19, at least 23 cases of Salmonella Braenderup in 9 states had been identified. Rose Acre Farms and Cal-Maine Foods, Inc. recalled over 206 million eggs sold under various brand names. People should not eat, and restaurants and retailers should not serve or sell, recalled eggs. The investigation is ongoing.
CDC provided technical assistance to the Nigeria Center for Disease Control for an outbreak of Lassa fever, a potentially life-threatening disease found in much of West Africa. Nigeria experiences annual increases in Lassa fever cases during the dry season, but this year’s outbreak caused great concern due to its size and geographic spread during the early months. From early January, when the outbreak began, to April 15, a total of 413 confirmed cases and 105 deaths had been reported.However, the reported numbers of cases and deaths have been declining in recent weeks.
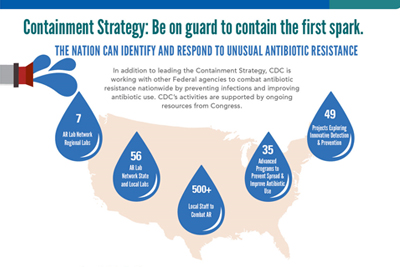
More than 23,000 Americans die each year from infections caused by germs resistant to antibiotics. While antibiotic resistance (AR) threats vary nationwide, AR has been found in every state. And unusual resistance germs, which are resistant to all or most antibiotics tested and are uncommon or carry special resistance genes, are constantly developing and spreading. Lab tests uncovered unusual resistance more than 200 times in 2017 in “nightmare bacteria” alone. Learn more in the current issue of Vital Signs.

Since November, CDC has been providing technical assistance to the South Africa National Institute for Communicable Diseases (NICD) on the world’s largest known outbreak of listeriosis. The outbreak has led to almost 1,000 illnesses and more than 180 deaths since January 2017. NICD conducted interviews of sick people, and product and environmental testing, and found that the outbreak was linked to polony, a type of processed meat.

Approximately 130 people die from rabies in Haiti each year. CDC is working with the Haiti Ministry of Agriculture to prevent more deaths by improving dog vaccination coverage. More than 210,000 dogs have been vaccinated against rabies since the campaign kicked off in October 2017. CDC and partners are utilizing a new strategy, which uses mobile phones to provide daily direction to rabies vaccinators and to track vaccinated dogs.

CDC has closed its investigation of a multistate outbreak of multidrug-resistant Salmonella Heidelberg infections linked to bull calves. A total of 56 people in 15 states were infected with Salmonella linked to dairy calves. Illnesses could continue because people may not know they could get a Salmonella infection from contact with dairy calves or other cattle. It is important to take steps to stay healthy around cattle.

Last month, CDC and public health laboratory partners transitioned from pulsed-field gel electrophoresis (PFGE)—used for the past 20 years—to whole genome sequencing (WGS) to conduct outbreak surveillance of Listeria. Since 2013, a nationwide Listeria pilot using WGS resulted in more outbreaks being detected with fewer cases compared with older methods like PFGE. Disease detectives identified foods like ice cream, frozen vegetables, and caramel apples as outbreak sources; this information helped to make these foods safer for the public.

Raw (unpasteurized) milk has been linked to many foodborne illnesses, including Campylobacter infections. Find out what happened after public health investigators learned of people becoming sick after drinking raw milk distributed through a herdshare program in Colorado.

CDC and state and federal partners are investigating a multistate outbreak of Salmonella infections linked to frozen shredded coconut. On January 3, 2018, Evershing International Trading Company recalled all 16 oz. bags of Coconut Tree Brand frozen Shredded Coconut.
CDC recommends retailers not sell, restaurants not serve, and consumers not eat recalled product.
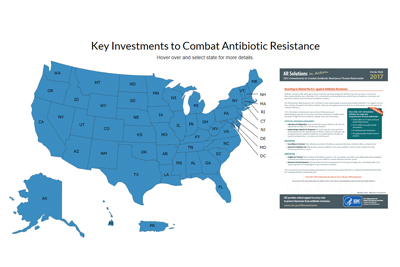
On January 10, CDC released new data in its Antibiotic Resistance (AR) Investment Map showcasing CDC’s activities to slow antibiotic resistance and meet national goals. The updated map for 2018 includes more than 170 state-reported successes in addressing AR problems. These are the first comprehensive reports on state progress made following the first year of Congress’s unprecedented investment in CDC’s Antibiotic Resistance Solutions Initiative. The map also features printable state- and city-specific fact sheets that describe how CDC invests in activities in those areas.