Our Work: 2017
Our Work - 2017

CDC staff deployments related to health issues caused by the three hurricanes continue in Houston, Puerto Rico, and the US Virgin Islands. In October, a CDC mycotics team helped the Texas Department of State Health Services investigate possible invasive mold infections associated with widespread flooding and indoor mold growth after Hurricane Harvey. Other staff have assisted the Puerto Rico Department of Health staff in identifying lab needs for clinical testing, and initiated a specimen transport system. This work enabled the public health lab to ship specimens to CDC and resume testing of priority pathogens. CDC epidemiologists helped lead the development of enhanced disease surveillance in Veterans Affairs (VA) health facilities in Puerto Rico. This collaboration between CDC and VA has provided crucial information about post-hurricane public health concerns on the island.
Still other CDC staff have been heavily involved with CDC’s Emergency Operations Center’s response to cases of leptospirosis in Puerto Rico and USVI following hurricanes Irma and Maria in September. CDC’s labs have been testing samples received from Puerto Rico since October 20, and confirmed and probable cases continue to be identified.

Two ongoing multistate Salmonella outbreaks remind us to always wash our hands after handling livestock, reptiles, and other animals. As of November 14, an outbreak of multidrug-resistant Salmonella Heidelberg infections linked to dairy calves has affected 54 people in 15 states. Additionally, as of November 16, a total of 66 ill people in 18 states had been reported in the multistate outbreak of Salmonella Agbeni infections linked to pet turtles.

In Bwabwata National Park, Namibia, a recent anthrax outbreak left more than a hundred lifeless hippopotami floating in the Okavango River. A CDC epidemiologist traveled to Namibia in October to assist with the outbreak investigation. A large number of Cape buffalo were also found dead and are undergoing testing for anthrax. So far these are the only species that have been identified as being affected.
As of November 14, more than 700 people have reportedly been exposed to the bacterium that causes anthrax. Most of these people received and have completed 14 days’ worth of ciprofloxacin for postexposure prophylaxis. For now, there have been no identified symptomatic human cases of anthrax (cutaneous or gastrointestinal). CDC continues to help Namibian health officials prevent further spread of the disease.

CDC marked the beginning of US Antibiotic Awareness Week on November 13 by launching Be Antibiotics Aware, an nationwide communication effort aimed at optimizing antibiotic prescribing among healthcare providers and educating patients and the public about appropriate antibiotic use. This important work dovetails with many CDC antibiotic resistance efforts, specifically the August launch of the Get Ahead of Sepsis educational effort.

Campylobacter outbreaks linked to puppies
Campylobacter (a type of bacteria) infections continue to be reported in the multistate outbreak linked to pet store puppies. As of October 23, a total of 67 people infected with Campylobacter infections were reported from 15 states. Regardless of where they are from, puppies might carry Campylobacter germs. CDC recommends people wash their hands with soap and water every time they touch a dog or its food, or clean up after a dog.
Innovations to stop emerging and zoonotic infections
A new CDC publication, Innovations to Stop Emerging and Zoonotic Infections, shines a light on some of CDC’s most cutting-edge technologies. It features stories about innovative technologies that have been vital in large outbreak responses as well as in tracking down more commonly seen illnesses caused by contaminated food or unclean water. Using plain language text and stunning images, it translates the work of CDC’s stellar scientists who have taken on challenges ranging from antibiotic resistance to Zika prevention.

CDC is closely monitoring an outbreak of plague in Madagascar and is providing technical assistance at the request of World Health Organization (WHO). CDC has sent personnel with expertise in infection prevention and control, vector control, border health, epidemiology, and plague. Although plague occurs there every year, the current outbreak is unusual because of reported person-to-person transmission in urban areas. At this time, CDC does not recommend that people avoid or postpone travel to Madagascar, but a level 2 travel alert has been posted, encouraging travelers to the country to take steps to prevent flea bites and avoid contact with sick or dead animals.

CDC awards $9 million to 25 investigators to combat antibiotic resistance
On October 23, CDC announced $9 million in awards for 25 projects to combat antibiotic resistance (AR) and improve patient safety. The results from this investment will help CDC protect people by detecting reservoirs of resistant germs, informing outbreak response, and preventing future infections. Focus areas include
- Discovering and evaluating new strategies that protect patients from resistance threats in healthcare settings.
- Investigating the human microbiome and pinpointing effective prevention strategies that protect people, their microbiomes, and the effectiveness of antibiotics.
- Examining the impact of antibiotic resistance in environmental settings, like surface water and soil, to determine potential downstream impacts on human health.
- The awards were made through a broad agency announcement (BAA) through the AR Solutions Initiative. In fiscal years 2016 and 2017, the AR Solutions Initiative awarded more than $24 million to BAA awardees.
Responding to recent hurricane emergencies

CDC staff have been supporting the federal response to hurricanes Harvey, Irma, and Maria in many ways. Staff from CDC’s National Center for Emerging and Zoonotic Diseases are serving in the field and in Atlanta, providing expertise in safe water and food, invasive fungal and bacterial infections, and communication. Other staff have traveled to Texas to support vector control efforts after Hurricane Harvey. NCEZID will continue to work with the agency’s Emergency Operations Center to support CDC’s response.
Engaging the public and healthcare providers about sepsis
Sepsis is a devastating condition that affects at least 1.7 million people each year in the US and causes nearly 270,000 deaths. Get Ahead of Sepsis, a CDC national educational effort to protect Americans from the devastating effects of sepsis, calls on healthcare professionals to educate patients, prevent infections, suspect and identify sepsis early, and start sepsis treatment fast. In addition, patients and their families are urged to prevent infections, be alert to the symptoms of sepsis, and seek immediate medical care if sepsis is suspected or for an infection that is not improving or is getting worse. Read the newly released article, “Incidence and Trends of Sepsis in US Hospitals Using Clinical vs Claims Data, 2009 – 2014,” in JAMA.
CDC works with global partners to fight cholera in Cameroon

Over the past few decades, Cameroon has faced several outbreaks of cholera. From 2011 to 2014 alone, the country reported 26,621 cases of cholera leading to 1,031 deaths. CDC is working with Cameroon, the World Health Organization and other partners to fight cholera and prevent another outbreak of the waterborne disease in the country. CDC and partners are working to deliver oral cholera vaccine to people in Cameroon’s at-risk areas. Earlier this year, a CDC staff member went to Cameroon for five weeks to help the country distribute more than 278,000 doses of vaccine.
A new One Health publication
More than half of all infections that people get are spread by animals. CDC’s One Health Office recognizes that the health of people is connected to the health of animals and our shared environment. Find out what the One Health Office has been up to recently by checking out their newest fact sheet. Learn more about their work in the United States and around the world to protect the health of people, animals, and the environment.
I am text block. Click edit button to change this text. Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
New Lyme disease study

CDC and Colorado State University scientists have identified a way to distinguish Lyme disease from a similar condition using an innovative approach, according to a study published August 16 in Science Translational Medicine. The findings are noteworthy because current laboratory tests for early Lyme disease are not ideal. The researchers were able to distinguish between early Lyme disease and southern tick-associated rash illness using biomarkers that show us how the body reacts to these illnesses. This could be important in helping to more accurately detect early Lyme disease, which is crucial because the longer people wait for Lyme disease treatment, the higher their risk for more severe symptoms. The research team hopes the findings will lay the groundwork for other studies that could lead to improved early testing for Lyme disease.
Illnesses in Texas Linked to Raw Milk

CDC scientists confirmed a case in a pregnant woman whose only potential exposure to this strain of bacteria (known as RB51) was through drinking raw milk from a nearby farm. Other people nearby also have symptoms consistent with RB51 infection. Milk from the farm also tested positive for RB51 and was recalled. CDC and Texas health officials have been contacting more than 800 households that may have purchased raw milk at the dairy between June 1 and early August. CDC and Texas are warning people about the need to see their doctor for antibiotics to prevent long-term symptoms of brucellosis. RB51 is used to vaccinate cattle against types of Brucella that are more dangerous to animals and to people. In rare circumstances, cows vaccinated with RB51 may shed the bacteria in milk.
$77M to states combat antibiotic resistance (AR)

In early August, through the Epidemiology and Laboratory Capacity for Infectious Diseases (ELC) cooperative agreement, CDC made $77M in investments nationwide for activities to combat AR. These funds help every state health department fight local resistance in foodborne infections and infections in healthcare facilities and communities. Supported by CDC’s AR Solutions Initiative, these investments include enhancements to the new AR Lab Network, including
- Increasing testing nationwide for the fungal threat Candida
- Adding a new national lab to conduct molecular testing on all US TB isolates
- Enhancing detection of resistant gonorrhea with whole genome sequencing
- Testing for “nightmare bacteria” CRE and performing whole genome sequencing on food and waterborne bacteria in every public health lab
Salmonella outbreak linked to papayas

CDC is investigating a multistate outbreak of Salmonella infections linked to Maradol papayas imported from Mexico. As of September 1, there have been 201 cases reported from 23 states; 65 ill people have been hospitalized, and one person from New York City died. Among 196 ill people with available information, 101 (66%) are of Hispanic ethnicity. Whole genome sequencing has been an important part of this investigation by showing the close genetic relatedness between Salmonella bacteria from ill people and those from papayas and by helping to determine who is part of the outbreak. CDC and FDA are advising consumers not to eat Maradol papayas from the Carica de Campeche farm located in Mexico. These papayas are sold under different brand names. The investigation is ongoing.
I am text block. Click edit button to change this text. Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
New data link outbreaks to fish
Fish continue to be an important source of foodborne outbreaks, according to a CDC study, “Fish-Associated Foodborne Disease Outbreaks: United States, 1998-2015,” published in early July in Foodborne Pathogens and Disease. About 260,000 people in the United States get sick from contaminated fish each year. Norovirus and Salmonella caused the largest outbreaks, and most outbreak-associated illnesses were caused by scombrotoxin, Salmonella, and ciguatoxin. The types of fish most often linked to outbreaks were tuna (37%), mahi-mahi (10%), and grouper (9%). Upstream control measures targeted to the most common causes and controls during processing and preparation could help reduce outbreaks caused by fish, according to the study.
Salmonella outbreaks linked to backyard poultry

Since June 2017, CDC has been investigating outbreaks of Salmonella infections linked to live poultry in backyard flocks. As of July 7, a total of 10 outbreaks involving 790 ill people in 48 states and Washington DC have been reported to CDC. The current number of ill people is higher than the 493 reported at this time last year, a reminder that Salmonella infections from backyard flocks continue to be a public health problem. Handwashing and other safe practices can help prevent illness.
Zika Update

Zika response activities in CDC’s Emergency Operations Center continue at a busy pace. Among recent highlights are four Zika-related MMWR articles coauthored by CDC scientists and released during June-July. These include reports on Zika prevention measures in Puerto Rico, pregnancy outcomes after maternal Zika virus infection in US territories, evaluation of placental and fetal tissue specimens for Zika virus infection, and updated CDC Zika testing guidance for pregnant women exposed to Zika. The four articles (there now have been 61 Zika MMWR reports since the response began in January 2016) offer a snapshot of the outstanding scientific contributions the response is making to further our understanding of this complex emerging infection.
Expanding antibiotic stewardship into rural areas

On July 14, CDC, in partnership with The Pew Charitable Trusts, the American Hospital Association, and the Federal Office of Rural Health Policy, released a new resource, Implementation of Antibiotic Stewardship Core Elements at Small and Critical Access Hospitals, on July 14. This guide adapts the CDC Core Elements of Hospital Antibiotic Stewardship Programs into practical ways that small hospitals, particularly critical access hospitals, can initiate and expand antibiotic stewardship activities in rural areas. It prepares facilities to address and overcome some of the challenges they face with limited staffing and resources. Providers who practice in these unique healthcare settings guided the development of this resource. CDC and its partners met with representatives from some of these facilities to better understand the challenges and get their input in developing materials that are more applicable and realistic to implement.
I am text block. Click edit button to change this text. Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
Ebola outbreak in the Democratic Republic of Congo
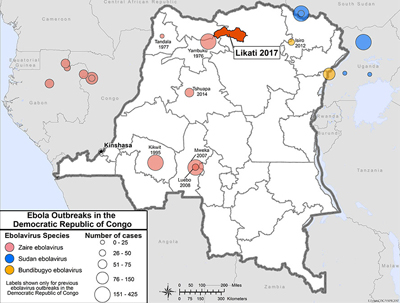
CDC staff have deployed to the Democratic Republic of Congo (DRC) to support the response to an outbreak of Ebola virus disease reported in the Likati Health Zone in northern DRC. They are providing support to the DRC Ministry of Public Health, the CDC country office, and other national and international responders. The outbreak began on April 22, after a 39-year-old man from the Nambwa Health area developed fever, vomiting, and bleeding, and then died in transit to the hospital. Two people who helped transport him later developed similar symptoms and died. As of May 30, the ministry reports 17 cases (12 suspected, 3 probable, 2 confirmed); 4 persons have died. The investigation is ongoing, and CDC will continue to assist in the response. VSPB health communications staff are engaging in regular discussions with CDC colleagues and international partners and providing educational and prevention materials about Ebola.
Zika update

As we move toward summer, CDC has ramped up activities to help prepare states for the 2017 mosquito season and potential cases of Zika. May saw an uptick in our efforts to get information out to state and local health departments to ensure they have the resources and information they need to respond to Zika this year. On May 5, we released an updated version of the CDC Zika Interim Response Plan based on lessons learned in 2016 and feedback from our state and local partners.
Zika is still a major public health concern, and CDC will continue working with the goal of protecting pregnancies from harm caused by infections with this virus.
2018 Yellow Book now available
The 2018 edition of the CDC Health Information for International Travel (commonly called the Yellow Book) is now available in print. It provides the US government’s most current health guidelines and information for international travel, including pre-travel vaccine recommendations, destination-specific health advice, and easy-to-reference maps, tables, and charts.
The Yellow Book is published every 2 years as a reference for health professionals providing care to international travelers and is a useful resource for anyone interested in staying healthy abroad.
There’s an app for that!
CDC has been testing a new mobile phone app designed by the nonprofit Mission Rabies that helps track canine rabies vaccination campaigns in near-real time.
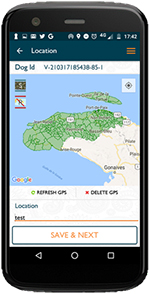
CDC’s rabies experts have been working to refine the app and to plan for the largest dog rabies vaccination campaign in Haiti. So far, the app has been helpful in tracking how the campaign is progressing. During the next phase starting May 21, the CDC rabies team will be using it to help direct where the vaccination teams should go to reach dogs that need vaccination. As of May 5, 41,500 dogs had been vaccinated, with an ultimate goal to have 800,000 dogs vaccinated nationwide by the end of July, which would be a 70% nationwide vaccination rate. If sustained for 5 years, this level is anticipated to disrupt rabies transmission. Rabies causes about 130 deaths in people annually in Haiti.
Updated guidelines for responding to pandemic flu
On April 21, HHS/CDC released a set of updated pre-pandemic planning guidelines entitled Community Mitigation Guidelines to Prevent Pandemic Influenza – United States, 2017. These guidelines replace the 2007 Interim Pre-pandemic Planning Guidance: Community Strategy for Pandemic Influenza Mitigation in the United States – Early, Targeted, Layered Use of Nonpharmaceutical Interventions (NPIs). The 2017 updated guidelines summarize key lessons learned from the 2009 H1N1 pandemic response, describe new or updated pandemic assessment and planning tools, and incorporate the latest scientific findings on the use of NPIs. In addition, six plain-language, pre-pandemic NPI planning guides are available online for different audiences and community settings. The supplemental guides can help states and localities operationalize the 2017 guidelines and assist them with pre-pandemic flu planning and decision-making. To access the updated guidelines, planning guides, and additional NPI communication, education, and training materials, please visit www.cdc.gov/npi.
New challenges in monitoring and preventing foodborne disease

Recent changes in the use of tests that diagnose foodborne illness pose challenges to monitoring illnesses and progress toward preventing foodborne disease, according to a report published April 20 in CDC’s Morbidity and Mortality Weekly Report. The MMWR article includes the most recent data from CDC’s Foodborne Diseases Active Surveillance Network, or FoodNet, which collects data on 15% of the US population. It summarizes preliminary 2016 data on nine germs spread commonly through food. In 2016, FoodNet reported 24,029 infections, 5,512 hospitalizations, and 98 deaths related to foodborne illness. Campylobacter and Salmonella caused the most reported bacterial foodborne illnesses in 2016.
New test to detect smallpox

In February, CDC’s Poxvirus and Rabies Branch received US Food and Drug Administration clearance for a diagnostic test to detect variola virus, the agent that causes smallpox. The new Variola Virus Real-time PCR Assay was designed to increase sensitivity and specificity and will replace the variola virus-specific test previously deployed to Laboratory Response Network (LRN) laboratories. The assay reagents and verification panels have been sent to qualified laboratories through the LRN. The deployment of the variola test enhances US government preparedness efforts to quickly detect and respond to a biological attack.
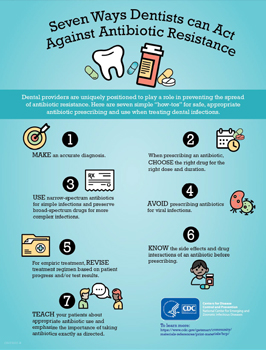
Dentists prescribe 10% of all antibiotic prescriptions in outpatient settings
Recent CDC study published in the Journal of the American Dental Association reported information about antibiotic prescribing among general dentists in the United States. The study found that although dentists usually prescribe within recommended guidelines, they sometimes prescribe antibiotics not indicated for dental conditions, such as fluoroquinolones and others used to treat urinary tract infections.
CDC’s Safe Healthcare Blog published Dr. Marie Fluent’s tips for supporting responsible antibiotic prescribing practices in dentistry. She is a dentist and educational consultant at the Organization for Safety, Asepsis, and Prevention.
Multistate outbreak linked to soy nut butter
CDC, FDA, and several states are investigating a multistate outbreak of 29 Shiga toxin-producing E. coli (STEC) O157:H7 infections reported from 12 states. Most of the sick people are children. The investigation has identified I.M. Healthy brand SoyNut Butter as the likely source of this outbreak. The SoyNut Butter Company recalled this product, as well as I.M. Healthy granola and Dixie Diner’s Club brand Carb Not Beanit Butter. CDC recommends that people not eat or serve these products. This investigation is ongoing.
Zika Update

Thirteen months into CDC’s Zika response, CDC continues to focus its efforts on reducing the risk of infections. CDC launched a series of eight 1-hour webinars to help state and local jurisdictions prepare for the 2017 Zika mosquito season. CDC also has updated its Zika travel guidance for pregnant women. CDC recommends that pregnant women not travel to areas where Zika virus has been newly introduced or reintroduced and mosquito-borne transmission is ongoing; areas where the virus was present before 2015 and there is no evidence transmission has stopped; and areas where the virus is likely to be circulating but has not been documented. This recommendation comes with a new World Map of Areas with Risk of Zika that allows users to search for location-specific Zika information and travel recommendations, and an interactive “Know Your Zika Risk” tool that offers tailored risk and prevention messages based on information provided by travelers.
A new analysis of Zika cases in Florida’s Miami-Dade County led CDC to alert residents of Broward and Palm Beach counties of a small potential increased risk of Zika virus transmission starting June 15, 2016. CDC recognized that people who regularly move between Miami-Dade, Broward, and Palm Beach counties may not realize they were traveling to an area with active mosquito-borne Zika virus transmission, and this movement between counties may pose a small but increased risk for Zika transmission. This increased risk is particularly relevant for Zika transmission via semen, because of evidence regarding the persistence of Zika virus in this reproductive tissue. Although blood donations in the United States are tested for Zika, there are no tests for tissue donors, including semen donors. CDC encourages women and their partners, in consultation with their healthcare providers, to consider this potential risk when trying to conceive.
Vaccine study to prevent monkeypox in DRC

A CDC-sponsored study to evaluate the effectiveness of Imvamune, a third-generation vaccine against smallpox, has begun. The study focuses on preventing infections from monkeypox virus, which is related to smallpox virus, in at-risk health care workers and laboratorians in Democratic Republic of Congo (DRC). The study has so far enrolled 24 participants in Kinshasa. In June, the second phase of the study will begin in Tshuapa, an area with a high risk of monkeypox infections among community members, placing healthcare workers at risk for infection. After smallpox eradication in 1980, countries around the world stopped regular vaccinations against the disease. Waning immunity to smallpox is thought to have contributed to the increased reports of monkeypox in Central and West Africa.
Investigating group A strep in Alaska

Teams from CDC’s Arctic Investigations Program partnered with state and local health officials in Anchorage, AK, to investigate and treat outbreaks of group A Streptococcus (group A strep) infection occurring in the homeless population there. CDC epidemiologists traveled to Anchorage in February to assist the Alaska Department of Health and Social Services with identification of risk factors for group A strep in the city’s homeless population. The CDC team helped implement and evaluate mass antibiotic treatment and infection control measures. An increase in the number of infections began in 2016 and has continued through the beginning of this year.
Outbreaks associated with imported foods

A small but increasing percentage of foodborne outbreaks in the United States is associated with imported food, according to an article authored by CDC scientists and published in a recent journal Emerging Infectious Diseases. From 1996 to 2000, imported food was linked to 1% of foodborne outbreaks, or about 3 outbreaks each year. From 2009 to 2014, imported food was linked to 5% of foodborne outbreaks, or about 18 outbreaks each year. Approximately 19% of food consumed in the United States is imported, including ≈97% of fish and shellfish, ≈50% of fresh fruits, and ≈20% of fresh vegetables. Knowing what imported foods are most often linked to outbreaks can help focus efforts to improve food safety and prevent future illnesses.
Learn about Salmonella and live poultry
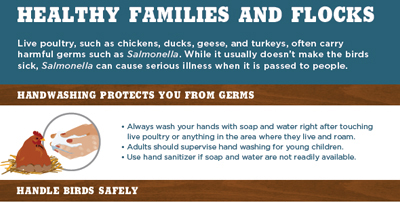
It’s spring, which means that many people are buying chicks and ducklings for backyard flocks. Yet backyard flocks can make their owners sick if proper precautions aren’t followed, as shown by the record number of Salmonella infections linked to backyard flocks in 2016. Before the spring selling season started, CDC distributed educational materials on preventing live-poultry-associated Salmonella illnesses to agricultural retail stores, hatcheries, and state agriculture department and health department collaborators.
CDC assists with cholera vaccination campaign

CDC is working with Cameroon’s ministry of health, the World Health Organization, and other partners on a cholera vaccination campaign targeting an estimated 130,000 people who live in Mogode District, bordering Nigeria in the Far North Region. This district has had multiple cholera outbreaks and has been the source of nationwide cholera epidemics in the past. The vaccine campaign is scheduled to take place in March and April, before the onset of the rainy season. CDC also assists Cameroon with other activities related to cholera preparedness, detection, and response through the Global Health Security Agenda.
Ebola virus detected in Ebola survivor 565 days after recovery

A team of CDC researchers recently published a study detailing the persistence of Ebola virus in the semen of a male survivor of Ebola virus disease. On August 27, 2014, Ebola virus was detected in the semen of a 48-year-old Ebola survivor in Liberia 565 days after his recovery from the Ebola. The patient also had a pre-existing HIV infection, which he was managing with treatment. While being treated for Ebola he continued his antiretroviral therapy regimen and was discharged from the Ebola treatment unit after his test came back negative for active Ebola virus infection. CDC researchers believe that the patient’s favorable response to the Ebola treatment despite being HIV positive could be linked to the patient’s compliance with his antiretroviral therapy regimen and adequate CD4 count. This emphasizes the importance of patients’ continuing their HIV treatment during an outbreak. The case highlights the need to continue researching the role that co-infections such as HIV and other causes of immunosuppression might play in the persistence of Ebola virus in male survivors of Ebola.
Frozen Shredded Coconut Linked to Outbreak

CDC and state and federal partners are investigating a multistate outbreak of Salmonella infections linked to frozen shredded coconut. On January 3, 2018, Evershing International Trading Company recalled all 16 oz. bags of Coconut Tree Brand frozen Shredded Coconut.
CDC recommends retailers not sell, restaurants not serve, and consumers not eat recalled product.