Emerging Infectious Diseases
Staying vigilant tracking emerging infectious diseases
CDC’s activities to protect Americans from emerging health threats are a foundation of many critical NCEZID infectious disease programs. NCEZID’s support for cutting-edge scientific research, public health programs, and outbreak response activities protect the United States from hundreds of dangerous viruses, bacteria, and mysterious organisms we have not yet identified.
NCEZID’s emerging infectious disease (EI) programs also provide fundamental support to the nation’s local, state, and territorial health departments.
EI programs are a top priority, critical to maintaining — and continually improving—surveillance, laboratory, and outbreak response capacity across the United States and around the world.
Melioidosis discoveries continue to surprise
NCEZID staff made a needle-in-a-haystack discovery in late 2021 when they linked four melioidosis cases (including two deaths) in four different states to a contaminated aromatherapy spray. This disease usually occurs in tropical climates, especially Southeast Asia and northern Australia, and can cause serious illness in people and animals. Treatment is difficult, and 10% to 50% of people infected with melioidosis die. Before 2022, nearly all melioidosis cases in the United States were among people who traveled outside the United States and were likely infected in places where the bacteria are more common.
In 2022, melioidosis threw another curveball. We discovered bacteria that cause melioidosis, Burkholderia pseudomallei, in soil and water along the Mississippi Gulf Coast. These bacteria were detected in the environment for the first time in the continental United States thanks to astute detective work by scientists investigating two melioidosis cases in southern Mississippi. Tests showed the bacteria that infected the two patients were genetically related, even though the illnesses occurred 2 years apart. NCEZID scientists and partners at the Mississippi Department of Health collected samples from both patients’ homes and then tested and sequenced them at CDC. Samples from soil and water around one of the homes tested positive for B. pseudomallei.
Climatic factors such as rising temperatures and precipitation could be making environmental conditions more favorable for pathogens like B. pseudomallei to expand into new areas. NCEZID’s increased support for its EI programs will bolster laboratory capacity to respond to emerging threats and strengthen the nation’s ability to prepare for, investigate, and respond to rare but dangerous illnesses like melioidosis.

Melioidosis is caused by infection with the bacteria Burkholderia pseudomallei.
ELC Leadership, Management, and Administration Project Investments
ELC funding to public health laboratories expands support through four leadership areas.*
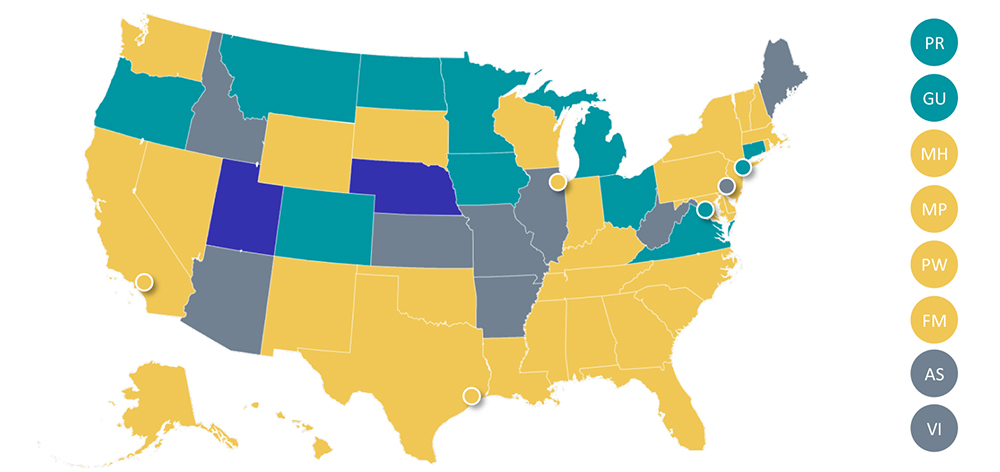
- Program leadership, including strategic direction and management
- Fiscal support to manage financial resources across the large ELC portfolio
- Administrative support to help manage programmatic reporting and activity monitoring
- Coordinating support to connect laboratory and epidemiology projects

Recipients with support in 3 key leadership areas filled

Recipients with support in 2 key leadership areas filled

Recipients with support in 1 key leadership area filled

Recipients with support in 0 key leadership areas filled
*The map above shows the number of key leadership areas filled through the ELC Cooperative Agreement by state. These investments are strongly influenced by recipient need as reflected in their ELC application and by availability of funds. None of the recipients has support in all four leadership areas.
Improving management of critical ELC resources
For more than 27 years, the Epidemiology and Laboratory Capacity for Prevention and Control of Emerging Infectious Diseases (ELC) Cooperative Agreement — and its 64-recipient state, large local, and U.S. territory and freely associated state health departments — have been critical to the nation’s infectious disease infrastructure. CDC’s ELC provides these recipients with financial and technical assistance to detect, prevent, and respond to emerging infectious diseases.
As the ELC cooperative agreement has grown so has the need for leadership and management in state and local health departments to support strategic planning and management. To address this need, ELC established the Leadership, Management, and Administration project in 2019, using NCEZID’s Emerging Infectious Disease funding and the Prevention and Public Health Fund. With this project, the ELC is helping health departments create infectious disease leadership that drives infectious disease readiness and response across a broad range of threats. This includes engagement and coordination across laboratory, epidemiology, and health information systems.
During the COVID-19 pandemic, staff in these leadership roles managed unprecedented funding levels and transformed these resources into impactful public health actions. The project has grown to 75 whole or partial positions across 51 of ELC’s 64 recipients. Expansion of this leadership project will help ensure all ELC recipients have the support needed to fortify U.S. health departments strategically and effectively.
Rare brain-eating ameba may be moving north
Naegleria fowleri is an ameba that lives in soil and warm fresh water, such as lakes, rivers, and hot springs.
Naegleria fowleri is an ameba that can cause a devastating brain infection called primary amebic meningoencephalitis (PAM). It is more commonly known as the brain-eating ameba. Since 1962, CDC has received reports of 157 people diagnosed with PAM in the United States; only four of them survived. The ameba usually infects people when contaminated water (often warm fresh water) enters through their nose.
In 2022, three children died from PAM. One became ill after swimming at a state park lake in Iowa, one after swimming in a small river in northeast Nebraska, and the third after swimming in a lake in Arizona. Until recently, PAM cases mostly occurred in the southern United States. However, since 2010, infections have been reported from more northern locations, suggesting the geographic range of Naegleria fowleri is expanding. Rising temperatures may be contributing to this change, as the ameba prefer to live in warmer waters. Expansion of disease surveillance systems, such as those supported by NCEZID’s emerging infectious disease programs, allows scientists to track dangerous infections like PAM and determine if they are increasing or changing due to our warming climate or other circumstances.
