Battling COVID-19
LEVERAGE existing platforms

Helping health departments tackle COVID-19
Each year, CDC awards millions of dollars through the Epidemiology and Laboratory Capacity for Prevention and Control of Emerging Infectious Diseases (ELC) Cooperative Agreement. This funding helps state, local, and territorial health departments detect, prevent, and respond to emerging infectious diseases. When the COVID-19 pandemic began, the US government relied on the existing ELC platform to equip health departments with the funding needed to respond. In FY 2021, ELC distributed nearly $31.6 billion, for a total of almost $43 billion since April 2020 to 64 state, local, and territorial health departments to assist with COVID-19 response efforts. Much of this funding supports critical activities that slow the spread of COVID-19 in communities across the country, including:
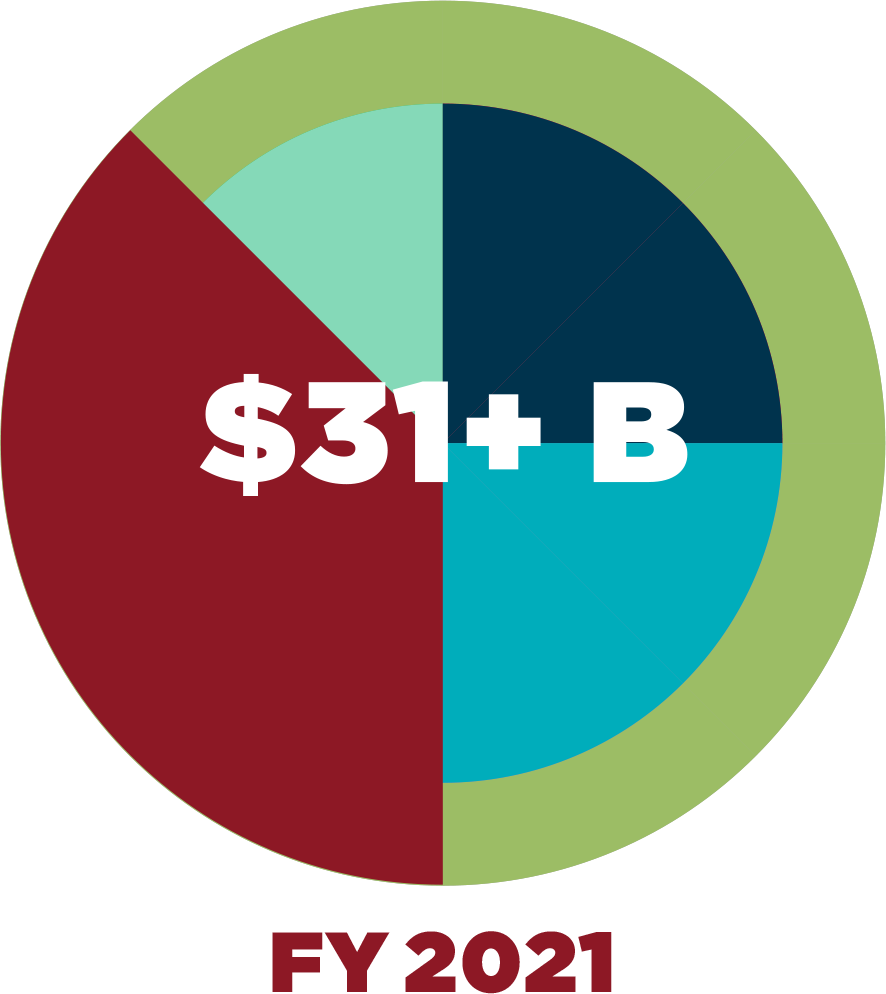
ELC funding awarded in 2021 was roughly 13,600% more than the funding awarded in 2019 to 64 state, local, and territorial jurisdictions.
• Testing
• Case investigation and contact tracing
• Improving disease surveillance systems
• Infection prevention and control
• Enhancing lab systems
CDC’s ELC program partnered with other federal agencies to support priority populations and locations. The ELC program partnered with the US Department of Education to implement a $10 billion initiative to support COVID-19 testing and other mitigation strategies in K–12 schools. Through a partnership with the US Department of Justice, ELC awarded $700 million to detect and stop the spread of COVID-19 in correctional and detention facilities, like jails and prisons. And, most recently, in collaboration with the US Department of Housing and Urban Development, CDC awarded $80 million to support COVID-19 detection and mitigation at service sites for people experiencing homelessness and at other congregate housing facilities.
ELC’s distribution of nearly $31.6 billion in FY 2021 provided critical funding to public health departments throughout the country to help detect and fight COVID-19.
Finding links from people to mink in the COVID-19 pandemic

The COVID-19 pandemic has had a surprising victim—mink. NCEZID staff and partners investigated mink deaths on farms in the US and found SARS-CoV-2 to be the culprit. The virus gives mink respiratory symptoms similar to those in humans. Investigations started in August 2020 with outbreaks on two farms in Utah, where staff from NCEZID’s One Health Office teamed up with colleagues from Utah’s departments of health and agriculture, CDC’s National Institute for Occupational Safety and Health, and the US Department of Agriculture. They found that before the mink died, the animals had contact with mink farm workers who had COVID-19.
Many diseases spread between people, animals, animal products, and the environment. The One Health Office specializes in these disease pathways and is studying them to understand how SARS-CoV-2 spreads. The mink investigations have expanded to testing wildlife and other animals like dogs and cats on and around mink farms. Fortunately, there is no evidence that animals are a significant source of SARS-CoV-2 transmission to people.
With CDC’s One Heath Office in place, we can continue to learn how diseases spread between animals and humans to help prevent future pandemics.
AMD initiates knowledge transfer

During the COVID-19 pandemic, public health scientists put advanced molecular detection (AMD) technology to work to identify the virus that causes COVID-19 and its emerging variants.
To help public health departments use this technology, NCEZID’s Office of AMD created the Technical Outreach and Assistance for States Team (TOAST). Through the agency’s COVID-19 response, the program collates protocols and develops training materials to support genomic surveillance of SARS-CoV-2 in a wide range of public health laboratories across the US.
TOAST identifies what type of support is needed and where tools can have the greatest impact. The program places a high priority on reducing barriers in genetic sequencing and data analysis by providing resources to laboratories at the state, local, and territorial levels. TOAST collaborated with researchers from the Centre for Genomic Pathogen Surveillance to conduct a broad analysis of the bioinformatics capacity, data systems, and reporting processes of public health laboratories within strategically identified sites. The results will be used to transform complex data into actionable information for public health leaders.
Boosting the power of state and local laboratories to conduct genetic sequencing and data analysis is vital in tracking variants of SARS-CoV-2 and other emerging pathogens.
BRIDGE gaps to help travelers stay safe
Planning travel in the time of COVID-19

People traveling around the US last year faced a series of decisions: Should I travel at all? How many infected people are at my destination? Will I need to be tested before I go? Will I need to wear a mask when I get there?
In response, CDC created the Travel Planner web portal. Users input their destination, or any stops along the way, and the portal provides information about travel restrictions or prevention policies the state, tribal, local, or territorial government has in place. Travelers have used the portal more than 1 million times to make informed decisions and reduce their risk of COVID-19 before, during, and after their trips.
The portal was designed in consultation with CDC partners, including the National Association of County and City Health Officials, the Council of State and Territorial Epidemiologists, the Association of State and Territorial Health Officials, and the Big Cities Health Coalition.
People traveling in the US accessed real-time information to better protect themselves from COVID-19 before, during, and after their trips.
Unifying data to monitor travelers at risk for infectious diseases
With millions of people traveling throughout the country daily, data about these travelers help CDC recognize the spread of dangerous infectious diseases that may be moving in, out, and around the country every day. But those data stretch across 20 large disparate systems. In 2021, CDC pulled all 20 data sets together into a single, secure platform called Synapse. This platform can be used to follow up with travelers who may have been exposed to concerning infectious diseases.
NCEZID’s Division of Global Migration and Quarantine modernized information systems used to respond to disease outbreaks at US ports of entry, such as seaports and airports. These systems include a near real-time data portal to monitor the volume and demographics of over 400 million annual international travelers. NCEZID also created a contact information exchange that provides states and territories with contact information for arriving international travelers so that they may conduct public health follow up. To date, Synapse has delivered secure data for more than 3.7 million travelers who were present in countries at high risk during the COVID-19 pandemic and travelers from countries with Ebola outbreaks.
A robust and secure travel data system helps CDC and partners control the spread of infectious diseases.
COLLECT data to guide action
Using valuable NHSN data collected from long-term care facilities

Early in the COVID-19 response, CDC’s National Healthcare Safety Network (NHSN) developed a Long-Term Care Facilities (LTCFs) COVID-19 module that enabled LTCFs to report vital data in a systematic way. As a result, all 15,400 US nursing homes certified by the Centers for Medicare & Medicaid Services (CMS) must now report the COVID-19 vaccination status and other valuable data collected from their 1.2 million residents and 1.8 million-plus staff. CDC works closely with CMS to use that information for infection prevention and control.
Using NHSN data, CDC determined that both vaccination and infection prevention strategies contributed to a 97% reduction in COVID-19 case rates in nursing homes since the peak in late December 2020. A subset of these data is now available on CDC’s COVID-19 Data Tracker, where COVID-19 cases and deaths among nursing home residents and nursing home staff members at the national and state levels are updated weekly. These data also informed decision-making about boosters in people residing in LTCFs as well as in the country at large.
Collecting data from long-term care facilities has been key to understanding how effective COVID-19 vaccines are at protecting people at increased risk for severe illness.
Detecting COVID-19 in wastewater

COVID-19 drove innovation across CDC. One result has been the development of wastewater testing as a bellwether for the spread of the disease.
Genetic material from SARS-CoV-2 ends up in wastewater through the feces of infected people. Tracking the amount of virus in wastewater systems can give authorities advance warning of new outbreaks and reliable trends of COVID-19 cases in communities. CDC’s National Wastewater Surveillance System (NWSS) is a unique collaboration among CDC, federal partners, state and local health departments, academic institutions, wastewater utilities, and private laboratories to help communities put this tool to work. By October 2021, test results for more than 22,000 wastewater samples were submitted to NWSS from systems that serve more than 41 million people.
Partners have used these data to confirm case spikes as the COVID-19 Delta variant surged across much of the US. In Ohio, for example, a statewide wastewater monitoring network now collects samples twice a week at 65 sewage-treatment plants and displays the results on its department of health website. CDC plans to expand the system to collect data on other infectious disease threats, such as antibiotic resistance and foodborne diseases.
Wastewater surveillance can detect evidence of COVID-19 in a community earlier than other surveillance methods.
