Outbreaks
Leading multiple outbreak responses
Outbreak preparedness and response is one of several core functions CDC’s National Center for Emerging and Zoonotic Infectious Diseases (NCEZID) employs to protect the public’s health. The center is uniquely equipped with hundreds of disease-specific, world-class experts; programs that crosscut all infectious diseases and agency responses; and extensive experience planning for and responding to infectious disease outbreaks in the United States and around the world, including outbreaks of fungal meningitis, Zika, and Middle East respiratory syndrome (MERS). Three years into the COVID-19 pandemic, and during the emergence of the global mpox outbreak, NCEZID continues to serve an essential role, leading response efforts to outbreaks ranging from Salmonella infections to Ebola.
Outbreak of Salmonella infections quickly linked to peanut butter

The investigation of a Salmonella outbreak that sickened people in 17 states resulted in the manufacturer recalling 49 peanut butter products, with another 21 recalls from companies that made products with the peanut butter.
CDC, several states, and the U.S. Food and Drug Administration (FDA) investigated an outbreak of 21 Salmonella infections in 17 states linked to peanut butter. In just 8 days, quick collaboration by investigators confirmed peanut butter as the source through interviews with people who were sick and sophisticated whole genome sequencing (WGS) analysis, including analysis of a 2010 FDA sample from a peanut butter manufacturing facility. Swift identification of peanut butter as the source prevented additional illnesses and limited the impact of the outbreak. WGS continues to be a revolutionary tool helping disease detectives find and solve outbreaks.

Peanut butter was contaminated with the bacteria Salmonella.
Preventing Ebola requires adding new tools to tried-and-true approaches

CDC microbiologist Sheny Morales-Betoulle (left) provides instructions before deactivating blood samples for Ebola antibody testing in Goma’s BSL3 (Biosafety) lab in the Democratic Republic of the Congo.
Back-to-back Ebola outbreaks—seven during the past 5 years with little reprieve between them—continue to spur NCEZID staff to action. Ongoing efforts aim to enhance lab capacity in affected countries, conduct trainings to sharpen disease detection skills among local public health workers, and partner with local organizations on culturally appropriate, community-based strategies for risk communication and community engagement.
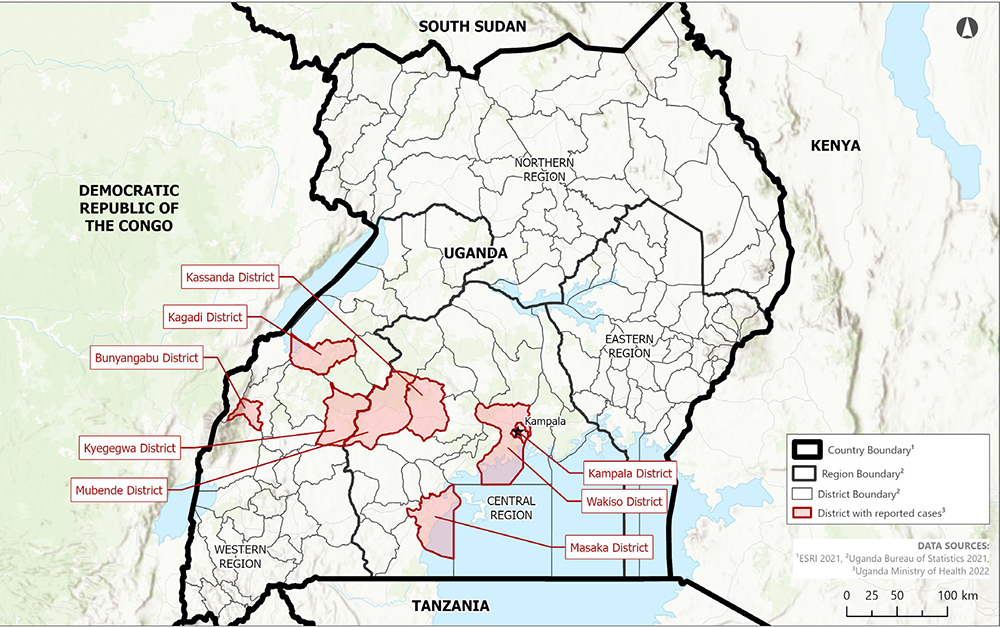
But as Ebola outbreaks continue to emerge, including the most recent outbreak caused by Sudan virus in Uganda, there is growing recognition that additional approaches are needed. In 2022, NCEZID launched a multicountry response effort that included blood sample testing (serosurveys), vaccine studies, and follow-up investigations of people who recovered from Ebola (survivor studies). Incorporating these newer tools, while continuing to bolster lab capacity and train local public health workers, will help us learn about the long-term effects of Ebola. It will also help us determine how long the Ebola vaccine provides protection, determine the potential for mild or asymptomatic infection, and understand causes of relapse in people who previously recovered from Ebola.
There is no single solution to controlling Ebola outbreaks. Quickly detecting and mitigating future outbreaks requires a commitment to interdisciplinary and novel approaches. Training and engaging laboratorians, epidemiologists, health educators, and communicators early is a critical priority to mitigate the effects of such frequent Ebola outbreaks.