2.1 Logic Models
‹View Table of Contents
Logic Models
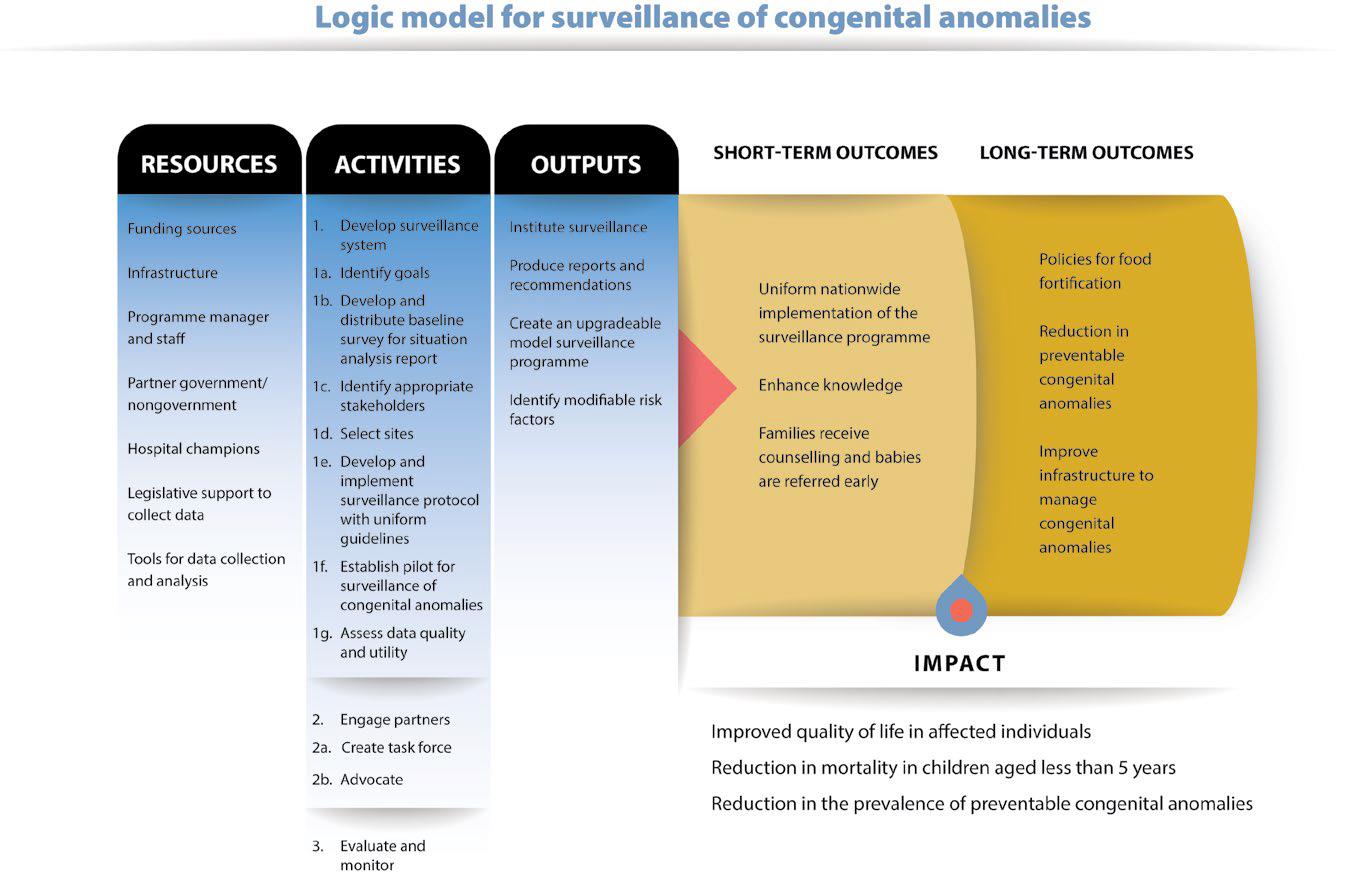
One approach that can be helpful when planning, implementing and evaluating a congenital anomalies surveillance programme is the use of logic models. A logic model is a graphic representation of how the surveillance programme will work. Logic models can identify what activities are needed, the order in which they would occur, and how the outcomes are going to be achieved.
Most often, logic models will include the following components:
- Resources: what resources currently exist? What resources will be required to build or expand a surveillance programme?
- Activities: what activities are required for the surveillance programme to function? Keep in mind that there might be more than one intended audience.
- Outputs: what are the expected outputs that will result from the activities?
- Expectations: what are the short-term, intermediate, and long-term expectations (or outcomes) for each programme area?
Logic models can have any shape (i.e. round, linear, columnar or a combination of these), and have any level of detail (i.e. simple, moderate or complex). It is probably best to begin by placing all relevant information into a table format (see Table 2.1) and then develop a logic model based on that information (see Fig. 2.1).
Creating a logic model has benefits. It can help define goals and objectives, as well as foster agreements among stakeholders about roles and responsibilities related to different activities. It can also help to identify gaps or barriers and build connections between activities and results. Please refer to Appendix D for another example of a logic model.
Table 2.1. Sample information to include in a logic model
| Resources | Activities | Outputs | Short-and long-term outcomes | Impact |
|---|---|---|---|---|
| Funding sources | 1. Develop surveillance system | Institute surveillance system | Uniform nationwide implementation of the surveillance programme | Improved quality of life for affected individuals |
| Infrastructure | 1a. Identify goals | Produce reports and recommendations | Enhance knowledge | Reduction in mortality in children aged less than 5 years |
| Programme manager and staff | 1b. Develop and distribute baseline survey for situation analysis report | Create an upgradeable model surveillance programme | Develop policies | Reduction in the prevalence of preventable congenital anomalies |
| Partner government/ nongovernment |
1c. Identify appropriate stakeholders | Identify modifiable risk factors | Improve need-based infrastructure to manage congenital anomalies | |
| Hospital champions | 1d. Select sites | |||
| Legislative support to collect data | 1e. Develop and implement surveillance protocol with uniform guidelines | |||
| Tools for data collection and analysis | 1f. Establish pilot for surveillance of congenital anomalies | |||
| 1g. Assess data quality and utility 2. Engage partners 2a. Create task force 2b. Advocate 3. Evaluate and monitor |
||||
| Adapted from: India team, Regional Workshop on Birth Defects Surveillance; Colombo, Sri Lanka, April 2012. | ||||