4.6 Orofacial Clefts
‹View Table of Contents
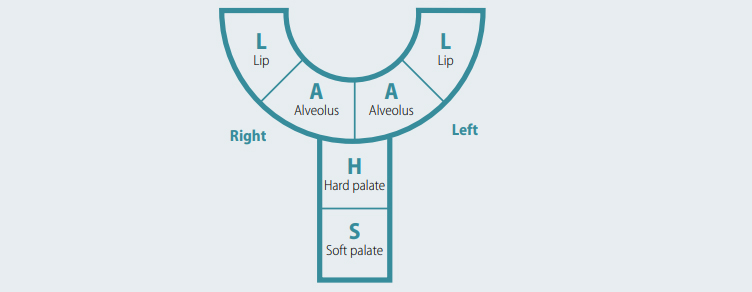
Cleft lip with or without cleft palate, and cleft palate alone, are collectively referred to as orofacial clefts. Descriptions for each of these conditions follow. To aid understanding of the individual conditions, the structure of a normal palate and the anatomy of a normal lip is shown above. Clefts should be coded using a single ICD code. For example, no infant should have a cleft only code plus a cleft lip code, but instead should have a single code for cleft lip and palate.
Some programmes might find it useful to provide more detail for certain conditions to aid in final diagnoses and for referral purposes. For orofacial clefts, many programmes use the LAHSAL system. LAHSAL is a simple method for describing and classifying oral clefts. One advantage of this system is that LAHSAL is often used by plastic surgeons to evaluate treatment outcomes.
LAHSAL (see Fig. 4.23) is an acronym for a sequence of descriptors:
Lip, right – Alveolus, right – Hard palate – Soft palate – Alveolus, left – Lip, left
The letters are read from the patient’s right to left.
Upper-case letters represent complete clefts: L
Lower-case letters represent incomplete clefts: l
No cleft is represented with a dot: .
An asterisk represents a microform cleft: *
CLEFT PALATE (Q35, Q35.1, Q35.3, Q35.5, Q35.59, Q87.0)
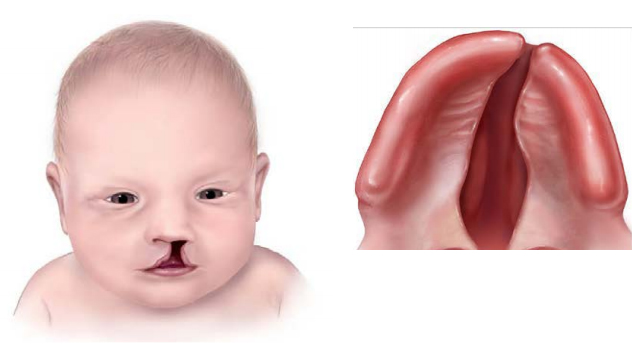
Cleft palate (also called palatoschisis) is characterized by a fissure in the secondary palate (posterior to the incisive foramen)and can involve the soft palate only or both the hard palate and the soft palate. The cleft can be narrow (V-shaped) or wider (U-shaped). The lip is intact. Laterality of cleft palate is difficult to ascertain and some believe it does not exist.
Cleft palate only (a term often used to refer to cleft palate with intact lip) is more often associated with additional birth defects and syndromes, so a careful physical examination with appropriate internal organ assessment is strongly recommended.
Fig. 4.22. Cleft palate, including hard and soft palate

Relevant ICD-10 codes
Q35.1 Cleft hard palate
Q35.3 Cleft soft palate
Q35.5 Cleft hard palate with cleft soft palate
Q35.59 Complete cleft palate
Q35.9 Cleft palate, unspecified
Q35 Cleft palate: Avoid using this generic code if more specific information is available
Related ICD-10 code
Q87.0 Robin sequence or defect, with core components including retro-micrognathia, posterior displacement of the tongue (glossoptosis) and respiratory obstruction. Cleft palate is a common though not required component of the Robin sequence. Whereas ICD-10 lists Robin sequence as an exclusion from the Q35 series, because it is such a common condition, the 87.0 code is suggested.
Notes:
- Q35 is the generic code for cleft palate. However, avoid using this code if more specific information is available.
- A simple alternative approach to classification and coding is the LAHSAL method, used often by plastic surgeons to assess for treatment outcomes (see Fig. 4.23). In surveillance it is best used in addition to, rather than instead of, the ICD codes.
Diagnosis
Prenatal. Cleft palate alone can be suspected prenatally, but it can easily be missed or misdiagnosed. Cases identified or suspected prenatally should be confirmed postnatally before inclusion in the surveillance programme.
Postnatal. Cleft palate can be missed at the external newborn examination if the palate is not systematically and carefully examined. This requires visualization of the entire length of the palate. When examining the palate, check for the presence of lower lip pits, which are a diagnostically useful sign of a specific autosomal dominant condition, and for signs of Pierre Robin sequence (microretrognathia, glossoptosis, respiratory obstruction). Clinically, a cleft palate might manifest with nasal regurgitation of feeds or difficulty feeding.
Clinical and epidemiologic notes
Photographs can be very helpful in uncertain or difficult cases, as they allow expert review, but good-quality images of a cleft palate might be difficult to obtain. Additional useful imaging techniques include CT and MRI.
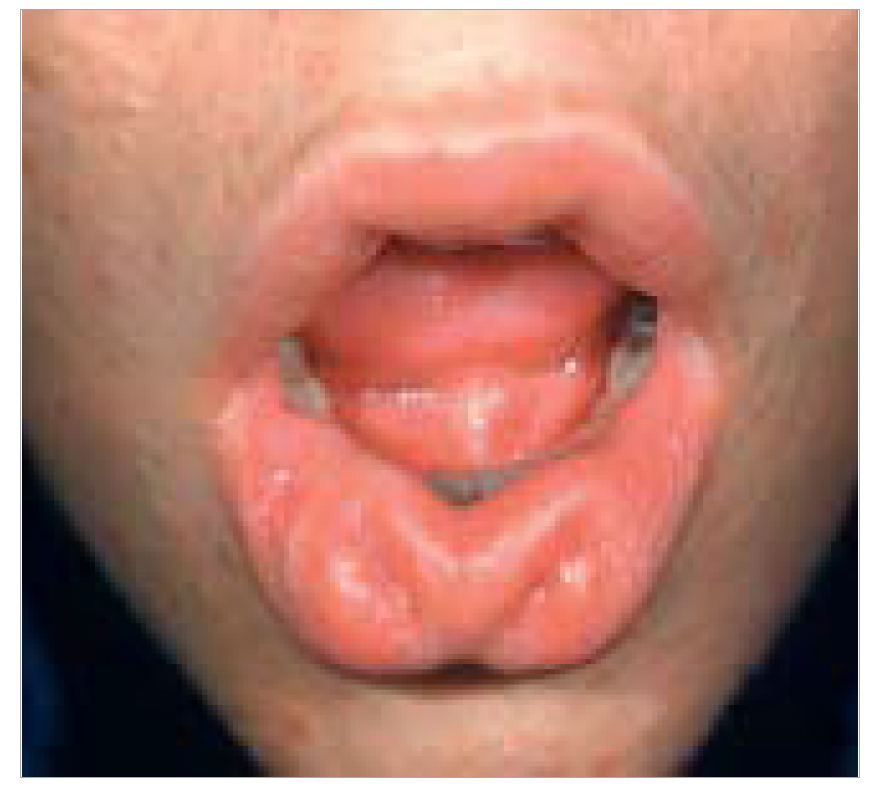
Be sure to note “lip pits” in the lower lip pits in the context of orofacial clefts (including cleft palate alone), which is indicative of the autosomal dominant condition van der Woude syndrome, and is the most common syndrome associated with otherwise apparently isolated clefts.
All orofacial clefts (cleft lip, cleft palate, and cleft lip with cleft palate) have similar non-genetic risk factors. Non-genetic risk factors for cleft palate include maternal smoking, drinking alcohol, use of some medications (selected seizure medications such as barbiturates, valproate and topiramate), obesity and high fever. Some suggested additional risk factors include pregestational diabetes, substances that are folic acid antagonists, and systemic steroids.
Cleft palate occurs with a birth prevalence of approximately 6 per 10 000 births (or ~1 in 1500 births), but with a very wide variation in different studies and populations. Outside of methodologic factors, the main factor in variability appears to be ethnicity, with higher prevalence in people of Northern European, Native American/First People, and Asian ancestry.
Inclusions
Q35 and subgroups except for Q35.7 (bifid uvula): Cleft palate (excluding bifid uvula and submucous cleft palate)
Exclusions
Q37 Cleft palate with cleft lip
Q35.7 Bifid (cleft) uvula
Q38.5 Absence of uvula
Submucous cleft palate: This defect is not a considered a major anomaly and should not be included in prevalence counts of cleft palate. Submucous cleft palate does not have a specific code.
Checklist for high-quality reporting
| Cleft Palate – Documentation Checklist |
Describe in detail, including:
|
Suggested data quality indicators
| Category | Suggested Practices and Quality indicators |
| Description and documentation | Review sample of clinical description for documentation of key descriptors.
|
| Coding |
|
| Clinical classification |
|
| Prevalence |
|
Fig. 4.23. LAHSAL
CLEFT LIP (Q36, Q36.0, Q36.9, Q36.90, Q36.99)
Cleft lip is characterized by a partial or complete fissure of the upper lip. It can be unilateral (Fig. 4.24, panels a, b) or bilateral (Fig. 4.24, panel c). In bilateral cleft lip, a median remnant of the philtrum is always present. The cleft lip can extend through the gum, but not beyond the incisive foramen. If the cleft extends further backwards into the secondary palate it becomes a different entity – a cleft lip with cleft palate.
Fig. 4.24. Cleft lip
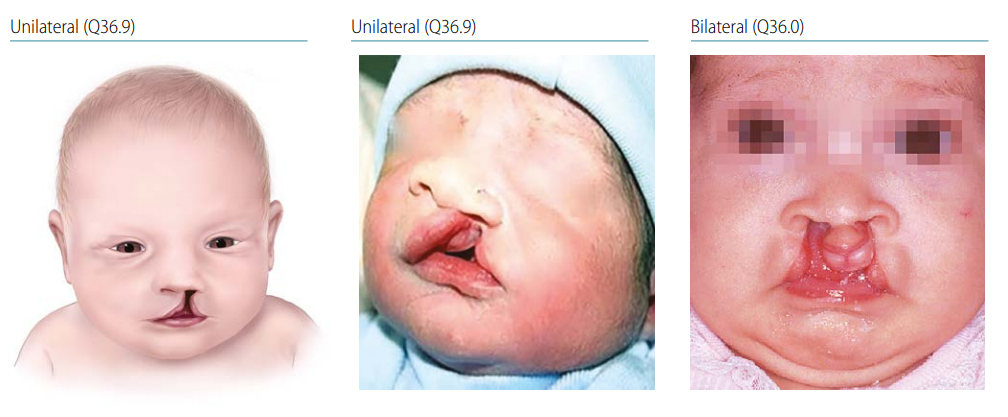
Photograph sources: (b) Dr Jaime Frías (EE. UU.); (c) Dr Pedro Santiago and Dr Miguel Yanez (EE. UU.). CLEFT LIP (Q36, Q36.0, Q36.9, Q36.90, Q36.99)
Rarer conditions that could be confused with typical cleft lip are median cleft lip (Q31.1) and atypical or Tessier type craniofacial clefts. Median cleft lip can be distinguished from bilateral cleft lip because in medial cleft lip there is no tissue below the philtrum (see below for more information on median cleft lip). In bilateral cleft lip (panel c) a midline remnant of tissue is always present. Atypical or Tessier type craniofacial clefts are a group of defects that involve clefts of the cranial and/or facial skeleton. Unlike cleft lip where the cleft extends up towards the nose, the 14 various Tessier’s clefts extend through radiating axes of facial and cranial bones, including towards the eye or nasolacrimal canal (oro-orbital or Tessier 5 cleft), or even more laterally towards the ear (oroauricular or Tessier 7 cleft). Both median and Tessier type clefts are much rarer than typical cleft lip.
Relevant ICD-10 codes
Q36.0 Cleft lip, bilateral
Q36.9 or Q36.90 Cleft lip, specified as unilateral
Q36.99 Cleft lip, unspecified
Note: Q36 is the generic ICD-10 code for cleft lip. However, avoid using this general code if more specific information is available.
Diagnosis
Prenatal. Cleft lip can be suspected prenatally, but it can easily be missed or misdiagnosed. Cases identified or suspected prenatally should be confirmed postnatally before inclusion in the surveillance programme.
Postnatal. Cleft lip is easily recognized on physical examination after delivery. The palate should be checked carefully to exclude the presence of cleft lip with cleft palate.
Clinical and epidemiologic notes
Older terms for cleft lip, no longer in use and best avoided, include cheiloschisis, congenital fissure of lip, harelip (pejorative), labium leporinum (pejorative).
Unilateral cleft lip is much more common than bilateral cleft lip. Left-sided cleft lip is more common than right-sided cleft lip.
Photographs can be very helpful in uncertain or difficult cases, as they allow expert review.
Microform cleft lip resembles a typical cleft lip that has healed prenatally, leaving what appears to be a scar where a cleft lip typically occurs (see Fig. 4.25). Microform cleft lip is not a major congenital anomaly and is typically excluded by most programmes.
In median cleft lip, there is no remnant of tissue (philtrum) in the area below the nasal septum. Median cleft lip is part of a condition called absent premaxilla and is often an external finding in holoprosencephaly, a severe brain malformation.
Absent premaxilla and holoprosencephaly are associated with genetic syndromes, including trisomy 13.
In addition to median cleft lip and Tessier type cleft, other atypical clefts occur, albeit rarely. Other atypical clefts include incomplete median cleft lip (which occurs in oro-facio-digital syndromes and hydrolethalus syndrome) and clefts that can be seen with amniotic band or limb-body wall spectrum anomalies (a disruptive event rather than a primary malformation).
Note any “lip pits” in the lower lip (see Fig. 4.26). This finding in the context of cleft lip (and also cleft lip and palate) is indicative of an autosomal dominant condition called van der Woude syndrome
Fig. 4.25. Microform (“healed” cleft lip)
Fig. 4.26. Lip pits

All orofacial clefts (cleft lip, cleft palate, and cleft lip with cleft palate) have similar non-genetic risk factors. Non-genetic risk factors for cleft lip include maternal smoking, drinking alcohol (especially binge drinking), obesity, fever, some medications (selected seizure medications), and diabetes. Folic acid or multivitamin supplement use has been associated with a moderately reduced risk of cleft lip (with or without cleft palate).
Cleft lip occurs with a birth prevalence of approximately 3.5 per 10 000 births (or approximately 1 in 3000 births). Prevalence has been reported as higher in some Asian groups and possibly lower in people of African ancestry.
Inclusions
Q36 Cleft lip: Avoid using this non-specific code in favour of more specific codes
Q36.0 Cleft lip, bilateral
Q36.9 or Q36.90 Cleft lip, specified as unilateral
Q36.99 Cleft lip, unspecified
Exclusions
Q36.1 Median cleft lip
Median cleft lip is different etiologically and epidemiologically; it should be excluded and assessed separately from typical cleft lip.
Q37–Q37.9 Cleft palate with cleft lip
Cleft palate with cleft lip is included in a separate group of orofacial clefts.
Microform cleft lip (or pseudocleft) is not a major malformation and is not included with cleft lip. There is no associated ICD-10 code for microform cleft lip.
Craniofacial clefts (Tessier type clefts) are different etiologically and epidemiologically. These rare defects should be excluded and assessed separately from cleft lip. Tessier clefts do not have a separate code and are best coded as Q75.8: “Other specified congenital malformations of skull and face bones”.
Checklist for high-quality reporting
| Cleft Lip – Documentation Checklist |
Describe in detail, including:
|
Suggested data quality indicators
| Category | Suggested Practices and Quality indicators |
| Description and documentation | Review sample of clinical description for documentation of key descriptors: Laterality, extension (in lip or palate), lip pits, premaxilla.
|
| Coding |
|
| Clinical classification |
|
| Prevalence |
|
CLEFT PALATE WITH CLEFT LIP (Q37, Q37.0-Q37.5, Q37.8, Q37.9, Q37.99)
Cleft palate with cleft lip is characterized as a cleft of the upper lip extending through the hard palate (primary and secondary palate) and might also extend through the soft palate (left panel).
Other conditions that can be confused with – and that need to be differentiated from – typical cleft palate with cleft lip are the atypical or Tessier type clefts and the amniotic band spectrum. Atypical or Tessier type craniofacial clefts are a group of defects that involve clefts of the cranial and/or facial skeleton. Unlike a typical orofacial cleft where the cleft extends up towards the nose, the 14 various Tessier clefts extend through radiating axes of facial and cranial bones, including towards the eye or nasolacrimal canal (oro-orbital or Tessier 5 cleft), or even more laterally towards the ear (oro-auricular or Tessier 7 cleft). Tessier type clefts are substantially rarer than cleft palate with cleft lip. Amniotic band spectrum can cause facial disruptions that involve both the lip and palate, and often include atypical skull and brain lesions (e.g. atypical encephaloceles).
Fig. 4.27. Cleft palate with cleft lip

Relevant ICD-10 codes (see quick reference table on the right for the most common forms)
Q37.0 Cleft hard palate with bilateral cleft lip
Q37.10 Cleft hard palate with cleft lip, specified as unilateral
Q37.19 Cleft hard palate with cleft lip, unspecified
Q37.2 Cleft soft palate with bilateral cleft lip
Q37.3 Cleft soft palate with unilateral cleft lip
Q37.4 Cleft hard palate and soft palate with bilateral cleft lip
Q37.5 Cleft hard palate and soft palate with unilateral cleft lip
Q37.59 Cleft hard palate and soft palate with cleft lip, unspecified
Q37.8 Unspecified cleft palate with bilateral cleft lip
Q37.9 Unspecified cleft palate with unilateral cleft lip
Q37.99 Cleft palate with cleft lip, unspecified
| Cleft Palate | |||
| Cleft lip | Hard | Hard and soft Unspecified | Unspecified |
| Bilateral | Q37.0 | Q37.4 | Q37.8 |
| Unilateral | Q37.10 | Q37.50 | Q37.90 |
| Unspecified | Q37.19 | Q37.59 | Q37.99 |
Notes:
- Q37 is the generic code for cleft palate with cleft lip. However, avoid using this code if more specific information is available.
- A simple alternative approach to classification and coding is the LAHSAL method, used often by plastic surgeons to assess for treatment outcomes (see notes for detail). In surveillance, it is probably best used in addition to, rather than instead of, the ICD codes.
Diagnosis
Prenatal. Cleft palate with cleft lip can be suspected prenatally, but it is easily missed or misdiagnosed. Cases identified or suspected prenatally should be confirmed postnatally before inclusion in the surveillance programme.
Postnatal. Cleft palate with cleft lip is easily recognized on physical examination after delivery, provided the palate is also checked carefully.
Clinical and epidemiologic notes
Though used mostly for cleft lip, older terms, no longer in use and best avoided, include cheiloschisis, harelip (pejorative) and labium leporinum (pejorative).
Photographs can be very helpful in uncertain or difficult cases (like differentiating between atypical clefts such as Tessier type craniofacial clefts or amniotic bands), as they allow expert review.
Photographs can also help reviewers detect “lip pits” in the lower lip. This finding in the context of cleft lip (and also cleft palate with cleft lip) is indicative of an autosomal dominant condition called van der Woude syndrome.
All orofacial clefts (cleft lip, cleft palate, and cleft palate with cleft lip) have similar non-genetic risk factors. Non-genetic risk factors for cleft palate with cleft lip include maternal smoking, drinking alcohol (especially binge drinking), obesity, fever, some medications (selected seizure medications), and diabetes. Folic acid or multivitamin supplement use has been associated with a moderately reduced risk of cleft lip (with or without cleft palate).
Cleft palate with cleft lip occurs with a birth prevalence of approximately 6 per 10 000 births (or approximately 1 in 1500 births). Prevalence has been reported as higher with Asian ancestry and possibly lower in people of African ancestry.
Inclusions
Q37–Q37.9 Cleft palate with cleft lip
Exclusions
Q36 and subgroups These include all types of cleft lip alone, including median cleft lip
Craniofacial clefts (Tessier type clefts) are different etiologically and epidemiologically. These rare defects should be excluded and assessed separately from cleft palate with cleft lip. Tessier clefts do not have a separate code and are best coded as Q75.8: “Other specified congenital malformations of skull and face bones”.
Amniotic band spectrum is coded as Q79.80 (congenital constriction bands). Be sure to note all affected parts of the body.
Checklist for high-quality reporting
| Cleft Palate with Cleft Lip – Documentation Checklist |
Describe in detail, including:
|
Suggested data quality indicators
| Category | Suggested Practices and Quality indicators |
| Description and documentation | Review sample of clinical description for documentation of key descriptors: Laterality, extension (in lip or palate), lip pits.
|
| Coding |
 Example: The findings illustrated in the photograph (left-sided cleft palate with cleft lip) would be coded as [. . H S A L] – indicating no cleft on the right side (. .), a cleft of hard and soft palate with cleft lip and alveolus on the left. |
| Clinical classification |
|
| Prevalence |
|
Table of Contents
- Chapter 4: Diagnosing and Coding Congenital Anomalies
- 4.1 List of Selected External and Internal Congenital Anomalies to Consider for Monitoring
- 4.2 Congenital Malformations of the Nervous System: Neural Tube Defects
- 4.2a Anencephaly
- 4.2b Craniorachischisis (Q00.1)
- 4.2c Iniencephaly (Q00.2)
- 4.2d Encephalocele (Q01.0–Q01.83, Q01.9)
- 4.2e Spina Bifida (Q05.0–Q05.9)
- 4.3 Congenital Anomalies of the Nervous System: Microcephaly
- 4.4 Congenital Malformations of the Ear
- 4.5a Overview Congenital Heart D: Prenatal Diagnosis and Postnatal Confirmation
- 4.5b Common Truncus (Q20.0)
- 4.5c Transposition of Great Arteries (Q20.3)
- 4.5d Tetralogy of Fallot
- 4.5e Pulmonary Valve Atresia (Q22.0)
- 4.5f Tricuspid Valve Atresia (Q22.4)
- 4.5g Hypoplastic Left Heart Syndrome (Q23.4)
- 4.5h Interrupted Aortic Arch (q25.21, Preferred; Also Q25.2, Q25.4)
- ›4.6 Orofacial Clefts
- 4.7 Congenital Malformations of the Digestive System
- 4.8 Congenital Malformations of Genital Organs Hypospadias (Q54.0–Q54.9)
- 4.9a Congenital Malformations and Deformations of the Musculoskeletal System: Talipes Equinovarus (Q66.0)
- 4.9b Congenital Malformations and Deformations of the Musculoskeletal System: Limb Reduction Defects/Limb Deficiencies
- 4.9c Limb Deficiency Amelia (Q71.0, Q72.0, Q73.0)
- 4.9d Limb Deficiency: Transverse Terminal (Q71.2, Q71.3, Q71.30, Q72.2, Q72.3, Q72.30)
- 4.9e Limb Deficiency: Transverse Intercalary (Q71.1, Q72.1, Q72.4)
- 4.9f Limb Deficiency: Longitudinal Preaxial (Tibia, Radius, First Ray) (Q71.31, Q71.4, Q72.31, Q72.5)
- 4.9g Limb Deficiency: Longitudinal Postaxial (Fibula, Ulna, Fifth Ray) (Q71.30, Q71.5, Q72.30, Q72.6)
- 4.9h Limb Deficiency: Longitudinal Axial Limb Deficiency – Split Hand and Foot (Q71.6, Q72.7)
- 4.10 Abdominal Wall Defects
- 4.11 Chromosomal Abnormalities