4.11 Chromosomal abnormalities
‹View Table of Contents
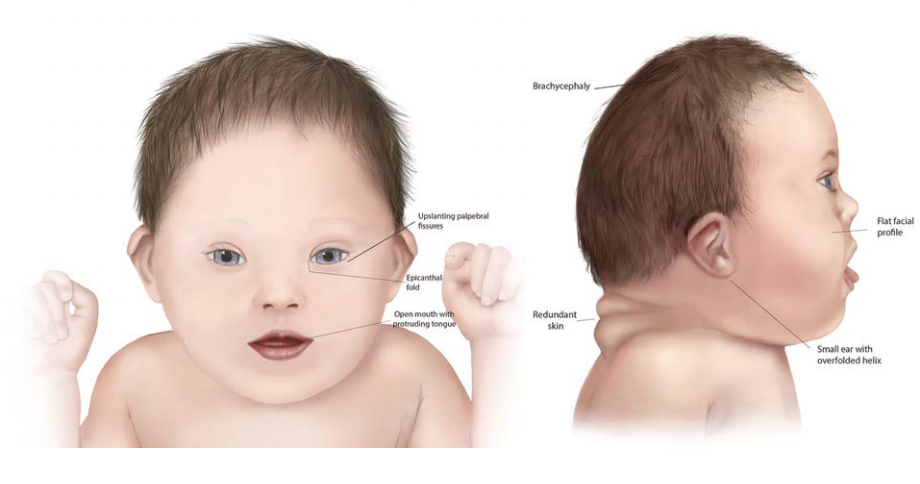
Trisomy 21, also known as Down syndrome, is a condition characterized by a distinctive pattern of minor and major anomalies associated with excess chromosome 21 material (see Fig. 4.44). About 95% of cases result from chromosomal non-disjunction, leading to each cell in the infant having three full copies of chromosome 21 (47,XX,+21 or 47,XY,+21) at conception. Rarer forms occur because of translocation, mosaicism or other chromosomal rearrangements/duplications. Translocation trisomy 21, accounting for about 2% of cases, is often familial, and commonly involves chromosomes 14 and 21. Mosaicism (concurrent presence of trisomy and normal cells) accounts for about 2% of cases. It results from post-zygotic non-disjunction or more rarely from trisomic rescue; that is, the loss in some cells of a chromosome 21 in a trisomic zygote. In the remaining 1% of cases, the extra chromosome 21 material originates from other rearrangements. The portion of chromosome 21 critical for the phenotype seems to be the 21q22 region.
Such classification is important for recurrence risk counselling, which varies by type of trisomy.
Fig. 4.44. Down syndrome
Relevant ICD-10 codes
Q90.0 Trisomy 21, nonmosaicism (meiotic nondisjunction)
Q90.1 Trisomy 21, mosaicism (mitotic nondisjunction)
Q90.2 Trisomy 21, translocation
Q90.9 Down syndrome, unspecified
Diagnosis
Prenatal. Trisomy 21 (Down syndrome) can be diagnosed through direct analysis of fetal chromosomes obtained from amniocentesis, CVS or percutaneous umbilical blood sampling. Because the placenta might contain mosaic cell lines not present in the fetus, mosaic trisomy 21 diagnosed through CVS should always be confirmed by a postnatal specimen from the infant. Analysis of fetal DNA in maternal blood can detect extra chromosome 21 material with high sensitivity and specificity, though it is still considered a screening test rather than a diagnostic test.
Postnatal. In most cases, Down syndrome can be strongly suspected or diagnosed clinically during the neonatal period by recognizing the typical physical traits. Clinical diagnosis should be confirmed by genetic testing (typically, karyotype from infant’s blood or tissue). The physical traits with greatest discriminant diagnostic value (in descending order) include the following (32):
- up-slanting palpebral fissures evaluated when the infant is crying
- flat nasal bridge
- decreased muscle tone (hypotonia)
- wider space between first and second toes (“sandal gap”)
- nystagmus
- brachycephaly
- incurving of the fifth finger (clinodactyly)
- narrow palate
- overfolded helix of the ear (especially with a small ear)
- short-appearing neck with redundant skin on the back of the neck
- broad and short hands and feet
- single transverse crease in the palm of the hand.
Clinical and epidemiologic notes
Major malformations associated with Down syndrome include some heart defects (in about 50%, most notably endocardial cushion defects), gastrointestinal atresias (duodenal or esophageal atresia), and vertebral abnormalities, among others.
Over time, infants with Down syndrome can present many other health and developmental issues, which need to be diagnosed, treated or prevented. These include hypothyroidism, diabetes, vision and hearing issues (e.g. cataracts) and intellectual disability of varying degree. Published clinical guidelines provide guidance for preventive and anticipatory health management.
Birth prevalence is approximately 1 in 1000 but varies depending on the maternal age profile of the population (the higher the age, the higher the frequency).
Inclusions
Q90.0 Trisomy 21, nonmosaicism (meiotic nondisjunction)
Q90.1 Trisomy 21, mosaicism (mitotic nondisjunction)
Q90.2 Trisomy 21, translocation
Q90.9 Down syndrome, unspecified (clinical diagnosis only)
Exclusions
Q92.9 Trisomy and partial trisomy of autosomes, unspecified
Q95.0 Balanced Robertsonian translocations involving chromosome 21
Checklist for high-quality reporting
| Trisomy 21 (Down syndrome) – Documentation Checklist |
Describe in detail:
Take and report photographs: Show clearly the side and front view of the face; can be crucial for review. Describe evaluations to find or rule out related and associated anomalies:
Document specialty consultations (e.g. genetics, cardiology). Report whether autopsy (pathology) findings are available and if so, report the results. |
Suggested data quality indicators
| Category | Suggested Practices and Quality Indicators |
| Description and documentation |
|
| Coding |
|
| Clinical classification |
|
| Prevalence |
|
Table of Contents
- Chapter 4: Diagnosing and Coding Congenital Anomalies
- 4.1 List of Selected External and Internal Congenital Anomalies to Consider for Monitoring
- 4.2 Congenital Malformations of the Nervous System: Neural Tube Defects
- 4.2a Anencephaly
- 4.2b Craniorachischisis (Q00.1)
- 4.2c Iniencephaly (Q00.2)
- 4.2d Encephalocele (Q01.0–Q01.83, Q01.9)
- 4.2e Spina Bifida (Q05.0–Q05.9)
- 4.3 Congenital Anomalies of the Nervous System: Microcephaly
- 4.4 Congenital Malformations of the Ear
- 4.5a Overview Congenital Heart D: Prenatal Diagnosis and Postnatal Confirmation
- 4.5b Common Truncus (Q20.0)
- 4.5c Transposition of Great Arteries (Q20.3)
- 4.5d Tetralogy of Fallot
- 4.5e Pulmonary Valve Atresia (Q22.0)
- 4.5f Tricuspid Valve Atresia (Q22.4)
- 4.5g Hypoplastic Left Heart Syndrome (Q23.4)
- 4.5h Interrupted Aortic Arch (q25.21, Preferred; Also Q25.2, Q25.4)
- 4.6 Orofacial Clefts
- 4.7 Congenital Malformations of the Digestive System
- 4.8 Congenital Malformations of Genital Organs Hypospadias (Q54.0–Q54.9)
- 4.9a Congenital Malformations and Deformations of the Musculoskeletal System: Talipes Equinovarus (Q66.0)
- 4.9b Congenital Malformations and Deformations of the Musculoskeletal System: Limb Reduction Defects/Limb Deficiencies
- 4.9c Limb Deficiency Amelia (Q71.0, Q72.0, Q73.0)
- 4.9d Limb Deficiency: Transverse Terminal (Q71.2, Q71.3, Q71.30, Q72.2, Q72.3, Q72.30)
- 4.9e Limb Deficiency: Transverse Intercalary (Q71.1, Q72.1, Q72.4)
- 4.9f Limb Deficiency: Longitudinal Preaxial (Tibia, Radius, First Ray) (Q71.31, Q71.4, Q72.31, Q72.5)
- 4.9g Limb Deficiency: Longitudinal Postaxial (Fibula, Ulna, Fifth Ray) (Q71.30, Q71.5, Q72.30, Q72.6)
- 4.9h Limb Deficiency: Longitudinal Axial Limb Deficiency – Split Hand and Foot (Q71.6, Q72.7)
- 4.10 Abdominal Wall Defects
- ›4.11 Chromosomal Abnormalities