Chapter 4.9a Congenital Malformations and Deformations of the Musculoskeletal System: Talipes Equinovarus (Q66.0)
‹View Table of Contents
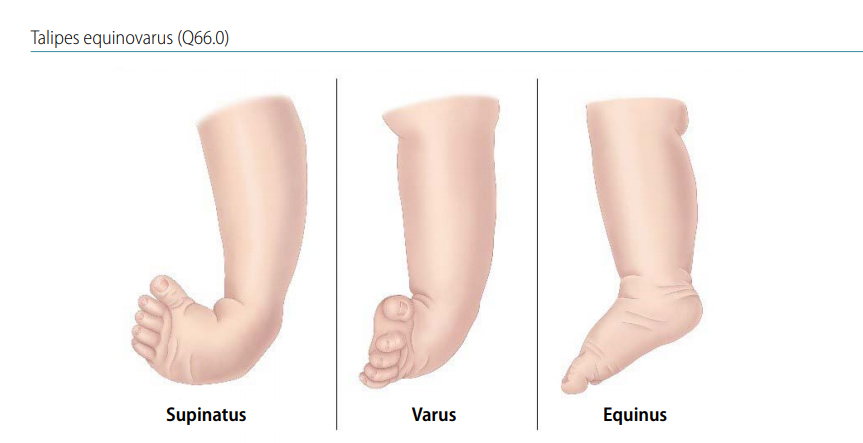
Talipes equinovarus (TEV) is a specific and common type of what is sometimes called “clubfoot”, a term that encompasses a range of anomalies of the ankle or foot present at birth (see Fig. 4.33). TEV can be defined as fixation of the foot (forefoot and hindfoot) in plantar flexion (equinus), deviation toward the midline (varus) and upward rotation so the foot rests on its outer side (supinatus). In other words, the foot points downward and inward and is rotated outward axially as shown in Fig. 4.34.
Fig. 4.33. Talipes equinovarus

Photograph and x-ray source: Dr Idalina Montes and Dr Rafael Longo (Puerto Rico).
Fig. 4.34. Foot positions
TEV has a wide spectrum of severity. In milder cases it is “positional”, meaning that it can be gently manipulated into a normal position and typically does not require orthopaedic or surgical interventions, and is excluded from birth defects surveillance. In more severe cases it can be “rigid” or “fixed”, in that it cannot be manipulated into a normal position and requires orthopaedic or surgical treatment, and is considered a major birth defect.
The most common congenital deformity of feet is TEV; however, there are other forms of clubfoot, specifically talipes calcaneovalgus (in which the ankle joint is dorsiflexed and the forefoot deviated outwards), and talipes calcaneovarus (in which the ankle joint is dorsiflexed and the forefoot deviated inwards).
Relevant ICD-10 codes
Q66.0 Talipes equinovarus
Q66.8 Other congenital deformities of feet, clubfoot NOS (not otherwise specified)
Q66.1 Talipes calcaneovarus
Q66.4 Talipes calcaneovalgus
Note:
Q66 Congenital deformities of feet: Avoid using this general code if more specific information is available.
Q66.8 Other congenital deformities of fee; Clubfoot NOS (not otherwise specified): Minimize the use of this code if possible; describe the anomaly so a more specific code (e.g. Q66.0) can be used.
Diagnosis
Prenatal. Clubfoot can be identified or suspected on prenatal ultrasound. However, it should not be included in birth defects surveillance data without postnatal confirmation. The primary utility of prenatal diagnosis of clubfoot is in its indication for additional evaluations for the genetic conditions and structural anomalies that are commonly associated with TEV.
Postnatal. Clubfoot is readily diagnosed in the newborn examination. Cases should be followed and evaluated sequentially to assess the degree of severity and whether treatment other than manipulation is necessary. Sometimes other birth defects of the foot or leg might mimic clubfoot. For example, a deficiency of the tibial bone in the leg might look like a talipes. Imaging studies (typically, radiographs) might provide supplemental information to aid in diagnosis.
Clinical and epidemiologic notes
TEV is bilateral in about 60% of cases, and when unilateral, TEV is slightly more common on the right side. Especially in the severe forms (fixed or rigid TEV), the calf muscles on the affected side are hypotrophic (smaller).
In about half of all cases, TEV occurs alone, or with other related musculoskeletal abnormalities such as torticollis, developmental dysplasia of the hip, and anomalies of multiple joints (e.g. arthrogryposis). TEV can occur with other birth defects, especially those affecting the brain and spine (e.g. spina bifida), through a mechanism thought to involve a deficit of innervation of the limb segments across joints that in turn leads to decreased movement in utero. Multiple deformations that include TEV can occur with genetic conditions that affect the formation of bones and joints (e.g. campomelic dysplasia, Larsen syndrome). More frequently, TEV can occur in chromosomal anomalies such as triploidy, deletion 4p-, and trisomies (though in trisomy 18, the type of clubfoot is calcaneovalgus, with dorsiflexion rather than plantar flexion of the foot).
Non-genetic risk factors reported to be associated with an increased risk for TEV include maternal smoking and possibly very early amniocentesis. In addition, the risk for TEV appears to be multifactorial, in that the recurrence risk for first-degree relatives is 3–6%, and the concordance in monozygotic twins is much higher than in dizygotic twins (30% versus approximately 3%).
The reported birth prevalence is 10–15 per 10 000 births, with moderate variability. Such variability is likely due in part to methodology (ascertainment, inclusion criteria), though ethnicity appears to play a role, with higher reported rates in certain groups (e.g. Maori, Polynesians, Australian Aborigines).
Inclusions
Congenital talipes equinovarus (including congenital, idiopathic, and neurogenic)
Talipes not otherwise specified, clubfoot not otherwise specified (minimize this group)
Q66.0 Talipes equinovarus
Q66.1 Talipes calcaneovarus
Q66.4 Talipes calcaneovalgus
Q66.8 Other congenital deformities of feet, Clubfoot NOS (not otherwise specified)
Exclusions
Clubfoot, positional (exclude; positional talipes is not considered a major defect)
Other presentations of congenital deformities of the foot (e.g. metatarsus varus or valgus, rocker-bottom foot, pes planus, pes cavus, etc.)
Checklist for high-quality reporting
| Talipes Equinovarus – Documentation Checklist |
Describe in detail, including:
|
Suggested data quality indicators
| Category | Suggested Practices and Quality Indicators |
| Description and documentation | Review sample of clinical description for documentation of key descriptors:
|
| Coding |
|
| Clinical classification |
|
| Prevalence |
|
Table of Contents
- Chapter 4: Diagnosing and Coding Congenital Anomalies
- 4.1 List of Selected External and Internal Congenital Anomalies to Consider for Monitoring
- 4.2 Congenital Malformations of the Nervous System: Neural Tube Defects
- 4.2a Anencephaly
- 4.2b Craniorachischisis (Q00.1)
- 4.2c Iniencephaly (Q00.2)
- 4.2d Encephalocele (Q01.0–Q01.83, Q01.9)
- 4.2e Spina Bifida (Q05.0–Q05.9)
- 4.3 Congenital Anomalies of the Nervous System: Microcephaly
- 4.4 Congenital Malformations of the Ear
- 4.5a Overview Congenital Heart D: Prenatal Diagnosis and Postnatal Confirmation
- 4.5b Common Truncus (Q20.0)
- 4.5c Transposition of Great Arteries (Q20.3)
- 4.5d Tetralogy of Fallot
- 4.5e Pulmonary Valve Atresia (Q22.0)
- 4.5f Tricuspid Valve Atresia (Q22.4)
- 4.5g Hypoplastic Left Heart Syndrome (Q23.4)
- 4.5h Interrupted Aortic Arch (q25.21, Preferred; Also Q25.2, Q25.4)
- 4.6 Orofacial Clefts
- 4.7 Congenital Malformations of the Digestive System
- 4.8 Congenital Malformations of Genital Organs Hypospadias (Q54.0–Q54.9)
- ›4.9a Congenital Malformations and Deformations of the Musculoskeletal System: Talipes Equinovarus (Q66.0)
- 4.9b Congenital Malformations and Deformations of the Musculoskeletal System: Limb Reduction Defects/Limb Deficiencies
- 4.9c Limb Deficiency Amelia (Q71.0, Q72.0, Q73.0)
- 4.9d Limb Deficiency: Transverse Terminal (Q71.2, Q71.3, Q71.30, Q72.2, Q72.3, Q72.30)
- 4.9e Limb Deficiency: Transverse Intercalary (Q71.1, Q72.1, Q72.4)
- 4.9f Limb Deficiency: Longitudinal Preaxial (Tibia, Radius, First Ray) (Q71.31, Q71.4, Q72.31, Q72.5)
- 4.9g Limb Deficiency: Longitudinal Postaxial (Fibula, Ulna, Fifth Ray) (Q71.30, Q71.5, Q72.30, Q72.6)
- 4.9h Limb Deficiency: Longitudinal Axial Limb Deficiency – Split Hand and Foot (Q71.6, Q72.7)
- 4.10 Abdominal Wall Defects
- 4.11 Chromosomal Abnormalities