5.2 Congenital Syphilis
‹View Table of Contents
Background
Syphilis is caused by the bacterium Treponema pallidum. The infection is most commonly transmitted through sexual contact (vaginal, oral or anal sex). Birth defects can occur in infants born to women who are infected with syphilis prior to or during pregnancy.
Main clinical manifestations in the mother
In primary syphilis, a sore or multiple sores appear at the site where the bacterium entered the body – typically near the genitals, the rectum or the oral cavity. The sores are usually firm, round and painless. In secondary syphilis, fever, swollen lymph nodes and skin rash, and wart-like genital lesions (condyloma lata) can be seen. In the latent stage, there are no signs or symptoms. In tertiary syphilis, several medical problems affecting the heart, neurologic system and other organs can be seen. Individuals with the infection move from one stage to the next in the absence of treatment.
Main clinical manifestations in the infant
Some infants with early congenital syphilis are asymptomatic at birth. Clinical manifestations of early congenital syphilis might include rhinitis (“snuffles”), hepatosplenomegaly, pustules on palms and soles, skin rash with desquamation, chorioretinitis and pigmentary chorioretinopathy (salt and pepper type), glaucoma, cataracts, interstitial keratitis, optic neuritis, periostitis and cortical demineralization of metaphysis and diaphysis areas of long bones, anaemia and thrombocytopenia (see Fig. 5.3). Some clinical signs consistent with congenital syphilis – such as hydrops and hepatosplenomegaly – might be detected by ultrasound during pregnancy. Infants who remain undiagnosed and untreated can progress to late congenital syphilis, resulting in numerous additional clinical manifestations, including, but not limited to: saddle nose due to destruction of cartilage, frontal bossing due to periostitis, tibial thickening (saber shins), joint swelling (clutton joints), perforation of hard palate, abnormal tooth development (Hutchinson’s teeth, mulberry molars), interstitial keratitis, neurologic deafness and optic nerve atrophy.
Fig. 5.3. Clinical findings in the infant

Typical desquamating and maculopapular skin lesions; punched out, pale, blistered lesions mainly on ears and nasal bridge, and desquamation of feet and palm.
Photograph source: Dr Ronald Ballard.

Rhinitis with mucopurulent nasal discharge
Photograph source: Dr Ronald Ballard.
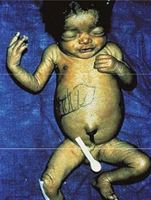
Hepatosplenomegaly and jaundice in an infant with congenital syphilis. Black markings on infant indicate liver margins.
Photograph source: Dr Ronald Ballard.
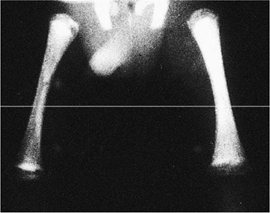
X-ray of bone abnormalities, syphilitic metaphysitis in an infant with diminished density in the ends of the shaft and destruction at the proximal end of the tibia (right).
Photograph source: Dr Ronald Ballard.
Diagnosis
Laboratory and radiography:
WHO recommends universal screening of pregnant women for syphilis. Diagnosis of congenital syphilis primarily relies on the diagnosis and treatment of the pregnant mother. Serum-based tests available for maternal diagnosis of syphilis include:
- rapid or laboratory-based treponemal tests (e.g. Treponema pallidum particle agglutination assay [TPPA]; Treponema pallidum hemagglutination assay [TPHA]; enzyme immunoassay [EIA]; chemiluminescence immunoassay [CLIA]); and
- non-treponemal tests (e.g. rapid plasma reagin [RPR] and venereal disease research laboratory [VDRL] tests).
Any of the following laboratory or radiography findings in the infant are consistent with a clinical diagnosis of congenital syphilis:
- demonstration of Treponema pallidum by darkfield microscopy; fluorescent antibody detection; immunohistochemical staining; or NAATs in the umbilical cord, placenta, nasal discharge or skin lesion material or autopsy material of a neonate or stillborn infant;
- cerebrospinal fluid (CSF) reactivity for VDRL test, and elevated CSF cell count or protein (without other possible cause);
- reactive non-treponemal serology titre (RPR or VDRL) in an infant that is fourfold or more than that of the mother at birth;
- reactive non-treponemal serology titre in an infant that is less than fourfold more than that of the mother but that remains reactive at least six months after delivery;
- long bone radiographs suggestive of congenital syphilis (e.g. osteochondritis, diaphyseal osteomyelitis, periostitis).
Case definition
Some children with congenital syphilis are born without clinical manifestation and many are not diagnosed at the time of birth. These can progress to late manifestations if left undiagnosed and untreated. To improve the diagnosis and treatment of infants who are undiagnosed at birth – leading to the prevention of long-term sequelae – WHO endorses a surveillance definition of congenital syphilis composed of two parts. Infants can be classified as cases of congenital syphilis based upon the diagnosis and treatment status of their mothers, as well as based upon their own laboratory and clinical findings.
The global surveillance case definition† for congenital syphilis is given below:
| 1. A live birth or fetal death (stillbirth) at > 20 weeks of gestation or > 500 g (including stillbirth) born to a woman with positive treponemal (TPPA, TPHA, EIA, IgM or rapid treponemal test) or non-treponemal (RPR, VDRL) syphilis serology and without adequate syphilis treatment. |
| 2. A live birth, stillbirth or child aged < 2 years born to a woman with positive syphilis serology or with unknown serostatus, and with laboratory and/or radiographic and/or clinical evidence of syphilis infection (regardless of the timing or adequacy of maternal treatment). (See laboratory diagnosis above.) |
† Surveillance case definitions might vary by country and available resources.
Relevant ICD-10 codes
A50.9 Congenital syphilis, unspecified
Q12.0 Congenital cataract
Q15.0 Congenital glaucoma
Checklist
- Examine the neonate for:
-
- Face: Rhinitis (snuffles) with mucopurulent nasal discharge.
- Skin: Jaundice, rash and desquamation, pustules on palms and soles.
- Abdomen: Hepatosplenomegaly (enlarged liver and spleen).
- Eye: Chorioretinitis and pigmentary chorioretinopathy (salt and pepper type), glaucoma, cataracts, interstitial keratitis, optic neuritis.
- Additional clinical examinations:
-
- Radiographs: Osteochondritis, diaphyseal osteomyelitis, periostitis.
- Hearing test: Hearing impairment (failed hearing screening must be followed with diagnostic testing to verify hearing loss)
- Obtain maternal medical health and pregnancy history for syphilis diagnosis.
- Collect maternal and neonatal blood samples for laboratory testing (maternal titres RPR or VDRL, neonatal blood count and thrombocytopenia).
- As indicated, test CSF for reactivity for VDRL test, or elevated CSF cell count or protein.
- Use darkfield microscopy or fluorescent antibody detection to detect Treponema pallidum in relevant tissue samples.
- Obtain photographs of the congenital anomalies observed.
- Record and report.