4.4 Congenital Malformations of the Ear Microtia: Anotia (Q16.0, Q17.2)
‹View Table of Contents
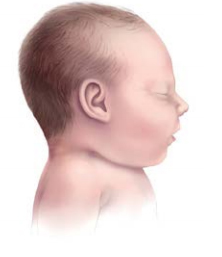
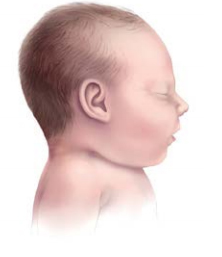
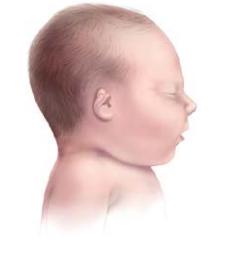
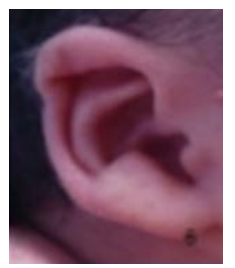
Fig. 4.13. Main types of microtia, including anotia
- Ear is small
- Ear canal may be narrowed
- Structures and ear shape are otherwise normal
- Ear is small
- Some components are missing
- Shape is markedly abnormal
- Ear is still recognizable

- Ear consists of a vertical mass of soft tissue and cartilage
- Typically associated with atresia of the externalcanal

- Most extreme and rarest form
- All external ear structures are absent



Microtia/anotia is a congenital malformation of the ear in which the external ear (auricle) is either underdeveloped and abnormally shaped (microtia) or absent (anotia). The external ear canal might be atretic (absent). The spectrum of severity in microtia ranges from a measurably small external ear (defined as longitudinal ear length more than two standard deviations below the mean, or approximately 3.3 cm in the term newborn) with minimal structural abnormality, to an ear that consists of few rudimentary structures and an absent or blind-ending external ear canal.
Based on morphology, microtia/anotia has been categorized (29) in the following four categories (see Fig. 4.13):
- First degree (type I), in which the external ear is small and the ear canal might be narrowed, but the structures and ear shape are otherwise normal (first-degree microtia is typically excluded in surveillance programmes because it does not have major health consequences).
- Second degree (type II), in which the ear is small, some components are missing so that the shape is markedly abnormal (resembling a hook, an S, or a question mark) but the ear is still recognizable.
- Third degree (type III), in which the external ear consists of a vertical mass of soft tissue with no resemblance to a normal auricle, typically associated with atresia of the external canal.
- Fourth degree or anotia (type IV), the most extreme and rarest form, in which all external ear structures are absent.
Microtia is usually unilateral (in which case it occurs more often on the right side). If bilateral, the severity can vary between the left and right sides.
Relevant ICD-10 codes
Q16.0 Congenital absence of (external ear) auricle (anotia, also known as fourth-degree microtia)
Q17.2 Microtia
Note that an additional digit could be added to specify the degree of microtia:
Q17.21 First degree (excluded in most programmes)
Q17.22 Second degree
Q17.23 Third degree
Diagnosis
Prenatal. Microtia/anotia is easy to miss prenatally. Delineating the position and shape of the ear might require three- dimensional ultrasound. Even if prenatal ultrasonography suggests microtia/anotia, the diagnosis should always be confirmed postnatally. When such confirmation is not possible – due, for example, to termination of pregnancy or unexamined fetal death – the programme should have criteria in place to determine whether to accept or not accept a case based solely on prenatal data.
Postnatal. Microtia/anotia can be easily recognized and classified based on the newborn physical examination. However, detection of middle and inner ear abnormalities, commonly associated with the more severe degrees of microtia, will require advanced imaging (CT or MRI scan), surgery or autopsy. Because microtia (second degree and above) is associated with hearing loss, hearing should be evaluated as soon as possible, ideally in the newborn period, so that appropriate management can be put in place.
Clinical and epidemiologic notes
Microtia/anotia is an isolated finding in 60–80% of infants. For this reason, it is crucial to report all findings and obtain good clinical photographs for expert review. Of note, microtia/anotia can occur in conjunction with other anomalies and syndromes, especially those involving the mandible and face. Such conditions include the oculo-auriculo-vertebral spectrum (OAVS) and Goldenhar“syndrome”(Q87.04), as well as genetic syndromes, such as Treacher-Collins syndrome (Q87.0A) and trisomy 18 (Q91.0), or teratogenic, such as retinoic acid embryopathy.
Non-genetic risk factors for microtia/anotia include maternal pregestational diabetes, and maternal use of isotretinoin (Accutane®), thalidomide or mofetil (CellCept®), taken periconceptionally or early in pregnancy.
The reported prevalence of microtia/anotia varies between 1 in 3000 to 1 in 20 000 births. The prevalence might vary by country and race/ethnicity but this is likely dependent on what forms of microtia are included in studies. Prevalence is reported to be higher in males than females.
Inclusions
Q16.0 Congenital absence of (external ear) auricle (anotia or also known as fourth-degree microtia)
Q17.2 Microtia
Q17.22 Microtia, second degree
Q17.23 Microtia, third degree
Exclusions
Small ear (microtia first degree) with normal auricle, including lop or cup ear Imperforate auditory meatus with a normal auricle, dysplastic or low-set ears
The following conditions in the absence of microtia/anotia (but code if microtia/anotia is present):
Q16.1 Congenital absence, atresia and stricture of auditory canal (external)
Q16.2 Absence of eustachian tube
Q16.3 Congenital malformation of ear ossicles
Q16.4 Other congenital malformations of middle ear
Q16.5 Congenital malformation of inner ear
Q16.9 Congenital malformation of ear causing impairment of hearing, unspecified
Q17.21 Microtia, first degree
H 90 Hearing loss
Checklist for high-quality reporting
| Microtia/Anotia – Documentation Checklist |
Describe in detail:
Take and report photographs: Show clearly the side and front; can be crucial for review. Describe evaluations to find or rule out related and associated anomalies:
Report whether autopsy (pathology) findings are available and if so, report the results. |
Suggested data quality indicators
| Category | Suggested Practices and Quality Indicators |
| Description and documentation | Review sample for documentation of key descriptors; severity (degrees second to fourth), laterality, presence of ear canal, preauricular tags or pits, lower lid coloboma, downslanting palpebral fissures:
|
| Coding |
|
| Clinical classification |
|
| Prevalence |
|
Table of Contents
- Chapter 4: Diagnosing and Coding Congenital Anomalies
- 4.1 List of Selected External and Internal Congenital Anomalies to Consider for Monitoring
- 4.2 Congenital Malformations of the Nervous System: Neural Tube Defects
- 4.2a Anencephaly
- 4.2b Craniorachischisis (Q00.1)
- 4.2c Iniencephaly (Q00.2)
- 4.2d Encephalocele (Q01.0–Q01.83, Q01.9)
- 4.2e Spina Bifida (Q05.0–Q05.9)
- 4.3 Congenital Anomalies of the Nervous System: Microcephaly
- ›4.4 Congenital Malformations of the Ear
- 4.5a Overview Congenital Heart D: Prenatal Diagnosis and Postnatal Confirmation
- 4.5b Common Truncus (Q20.0)
- 4.5c Transposition of Great Arteries (Q20.3)
- 4.5d Tetralogy of Fallot
- 4.5e Pulmonary Valve Atresia (Q22.0)
- 4.5f Tricuspid Valve Atresia (Q22.4)
- 4.5g Hypoplastic Left Heart Syndrome (Q23.4)
- 4.5h Interrupted Aortic Arch (q25.21, Preferred; Also Q25.2, Q25.4)
- 4.6 Orofacial Clefts
- 4.7 Congenital Malformations of the Digestive System
- 4.8 Congenital Malformations of Genital Organs Hypospadias (Q54.0–Q54.9)
- 4.9a Congenital Malformations and Deformations of the Musculoskeletal System: Talipes Equinovarus (Q66.0)
- 4.9b Congenital Malformations and Deformations of the Musculoskeletal System: Limb Reduction Defects/Limb Deficiencies
- 4.9c Limb Deficiency Amelia (Q71.0, Q72.0, Q73.0)
- 4.9d Limb Deficiency: Transverse Terminal (Q71.2, Q71.3, Q71.30, Q72.2, Q72.3, Q72.30)
- 4.9e Limb Deficiency: Transverse Intercalary (Q71.1, Q72.1, Q72.4)
- 4.9f Limb Deficiency: Longitudinal Preaxial (Tibia, Radius, First Ray) (Q71.31, Q71.4, Q72.31, Q72.5)
- 4.9g Limb Deficiency: Longitudinal Postaxial (Fibula, Ulna, Fifth Ray) (Q71.30, Q71.5, Q72.30, Q72.6)
- 4.9h Limb Deficiency: Longitudinal Axial Limb Deficiency – Split Hand and Foot (Q71.6, Q72.7)
- 4.10 Abdominal Wall Defects
- 4.11 Chromosomal Abnormalities