3.9 Potential Inclusion/Exclusion Criteria
‹View Table of Contents
To standardize the inclusion criteria for a case (fetus or neonate with a congenital anomaly) in a congenital anomalies surveillance programme, it is essential to characterize the criteria related to the diagnoses. Some examples of these criteria include the age at which the anomaly is diagnosed (discussed previously), the type of pregnancy outcome (discussed previously), the gestational age at delivery and birth weight, and maternal residence. More information about the latter two criteria follows.
Gestational age at delivery and birth weight are important components of the case definition, because the frequency of some congenital anomalies varies depending on these factors. For example, preterm and low-birth-weight babies have a higher frequency of patent ductus arteriosus and undescended testes than term infants, and these conditions are considered physiologically normal among preterm infants if they resolve within a short time frame without intervention. Please refer to the Glossary of terms for definitions of birth weight and gestational age.
The mother’s primary residence at the time of delivery or pregnancy termination is used by most congenital anomalies surveillance programmes to define the source population in which the cases occur. For example, residence can be defined as the mother’s primary address during the three months prior to pregnancy and the first trimester of pregnancy. This is important because residence and place at delivery may be different, particularly in areas with strong referral patterns. It is essential to focus on residence rather than place at delivery, in order to correctly identify the appropriate denominator (the population of births from which the cases derive) and numerator. Correct denominators and numerators are prerequisites for accurate monitoring of the prevalence of a congenital anomaly and monitoring of changes over time.
Examples of inclusion criteria for population-based surveillance
- Live births and fetal deaths (stillbirths):
- delivered with at least one of the selected major congenital anomalies (see Appendix A);
- delivered to a mother who resides within a catchment area;
- delivered at an age of 28 weeks’ gestation or more, or, alternatively, a birth weight of at least 1000 g when gestational age is not available, or with a gestational age defined by the programme. WHO recommends using an age of 28 weeks’ gestation or more or birth weight of at least 1000 g when gestational age is not available. However, each country can use its own standards, which will allow it to link with vital statistics data.
- The congenital anomaly may be diagnosed prenatally (and confirmed at birth), at birth, during the neonatal hospitalization period, or up to an age limit predetermined for case ascertainment.
- If follow-up of the infants is available in the country, then the surveillance programme could consider capturing infants within a defined time period, to include the follow-up period (e.g. up to 1 year after birth).
- If the site has the capacity to capture terminations of pregnancy, the programme can include those fetuses with at least one of the selected major congenital anomalies at any gestational age, for the subset of congenital anomalies for which a prenatal diagnosis is considered definitive (e.g. anencephaly). Each country will have different provisions to capture termination of pregnancies, but in many settings this is done by including prenatal diagnostic centres as potential case-finding sources.
- Programmes that are interested in more detailed information on inclusion of prenatal diagnosis in congenital anomalies surveillance can find some useful and practical suggestions and tips in the guidelines developed by the NBDPN in the USA (14).
Examples of inclusion criteria for hospital-based surveillance
- Live births and fetal deaths (stillbirths):
- delivered with at least one of the selected major congenital anomaly (see Appendix A)
- delivered at a participating hospital;
- delivered with an age of 28 weeks’ gestation or more, or, alternatively, a birth weight of at least 1000 g if gestational age is not available. The gestational age can be determined by each country, depending on its capacity to identify congenital anomalies occurring earlier than 28 weeks’ gestation.
- The congenital anomaly may be diagnosed prenatally (and confirmed at birth), at birth or during the neonatal hospitalization period. The usual hospitalization period after delivery varies among countries, but could be defined as up to seven days after birth.
- If the programme has the capacity to capture terminations of pregnancies, it can consider including those fetuses with at least one of the selected major congenital anomalies at any gestational age for the subset of congenital anomalies for which a prenatal diagnosis is considered definitive (e.g. anencephaly). Each country will have different provisions to capture termination of pregnancies, but in many settings this is done by including prenatal diagnostic centres as potential case-finding sources.
- Programmes that are interested in more detailed information on inclusion of prenatal diagnosis in congenital anomalies surveillance can find some useful and practical suggestions and tips in the guidelines developed by the NBDPN in the USA (14).
Examples of exclusion criteria for both population- and hospital-based surveillance
- All neonates who do not have one of the selected major congenital anomalies listed in the initial inclusion list (see Appendix A).
- All neonates – with or without congenital anomalies – of less than 28 weeks’ gestational age or with a birth weight of less than 1000 g, if gestational age is not available (or who are less than the gestational age or weight defined by the programme).
- All live births and fetal deaths with congenital anomalies identified outside of the participating hospital (hospital based) or outside of the ascertainment area (population based).
- Maternal residence status (the three months prior to pregnancy and the first trimester of pregnancy outside of the catchment area).
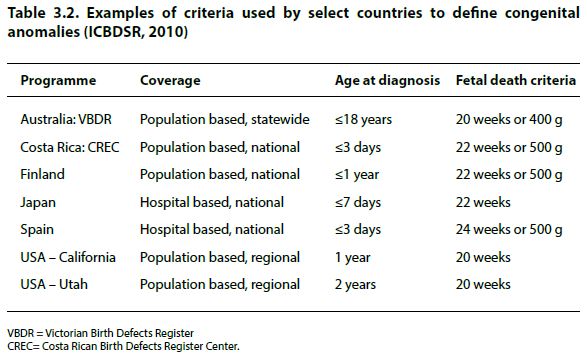
Table 3.2 gives examples of criteria used by different countries to define congenital anomalies.
After a programme has defined the inclusion and exclusion criteria, a standardized data collection process can be developed. This would include identifying the core ascertainment variables to be included in the surveillance programme and the development of a protocol for standardized data-collection procedures.
Table of Contents
- Chapter 3: Approaches to Surveillance
- 3.1 Population Coverage
- 3.2 Case Ascertainment
- 3.3 Case Finding
- 3.4 Case Inclusion
- 3.5 Description Formats for Congenital Anomalies
- 3.6 Age of Inclusion
- 3.7 Inclusion of Pregnancy Outcomes
- 3.8 Coding System
- ›3.9 Potential Inclusion/Exclusion Criteria
- 3.10 Core Ascertainment Variables
- 3.11 Data-Collection Methods and Tools
- 3.12 Data Management and Protocols
- 3.13 Data Collection and Management