2011 Salmonella Outbreak Linked to Ground Beef
NOTICE: This outbreak is over. The information on this page has been archived for historical purposes only and will not be updated.
Posted February 1, 2012
Outbreak Summary
CDC collaborated with public health officials in several states and the U.S. Department of Agriculture’s Food Safety and Inspection Service (USDA-FSIS) to investigate a multistate outbreak of Salmonella Typhimurium infections linked to eating ground beef purchased from Hannaford Supermarkets. Representatives from Hannaford cooperated with public health officials throughout the investigation. Public health investigators used DNA “fingerprints” of Salmonella bacteria obtained through diagnostic testing with pulsed-field gel electrophoresis (PFGE) to identify cases of illness that may have been a part of this outbreak. Investigators used data from PulseNet, the national subtyping network made up of state and local public health laboratories and federal food regulatory laboratories that performs molecular surveillance of foodborne infections. The outbreak strain of Salmonella Typhimurium was resistant to several commonly prescribed antibiotics. This antibiotic resistance may have been associated with an increase in the risk of hospitalization or possible treatment failure in infected individuals.
A total of 20 persons infected with the outbreak strain of Salmonella Typhimurium were reported from 7 states. The number of ill persons identified in each state was as follows: HI (1), KY (1), MA (1), ME (4), NH (6), NY (6), and VT (1). Among persons for whom information was available, illnesses began on or after October 8, 2011. Ill persons ranged in age from 1 year to 79 years old, with a median age of 45 years old. Fifty percent were male. Among the 17 ill persons with available information, 8 (47%) were hospitalized. No deaths were reported.
The outbreak can be visually described with a chart showing the number of people who became ill each day or week. This chart is called an epi curve. The PFGE pattern associated with illness in this outbreak has been seen before in PulseNet, and in the past typically caused 0-3 cases per month. Please see the Timeline for Reporting Cases of Salmonella Infection for more details.
Outbreak Investigation
Epidemiologic, traceback, and laboratory investigations conducted by officials in local, state, and federal public health, agriculture, and regulatory agencies linked this outbreak to eating ground beef purchased from Hannaford stores. Among 19 ill persons for whom exposure information was available, 14 (74%) reported consuming ground beef in the week before their illness began. This proportion is significantly higher than results from a survey of healthy persons in which 40% of persons interviewed reported consuming any ground beef at home in the 7 days before they were interviewed. Among the 14 ill persons who reported consuming ground beef, 12 (86%) reported purchasing ground beef from Hannaford stores. For ill persons for whom information was available, reported purchase dates ranged from October 12, 2011 to December 10, 2011. Product information (such as date and location of purchase of ground beef) was collected from ill persons and used by local, state, and federal public health, agriculture, and regulatory agencies to further the investigation.
Laboratory testing conducted by the State of Maine Health and Environmental Testing Laboratory and the New York State Department of Health, Wadsworth Center Laboratories isolated the outbreak strain of Salmonella Typhimurium from 2 separate samples of leftover ground beef purchased from Hannaford stores and collected from unrelated ill persons’ homes in Maine and New York.
This was a multidrug resistant strain of Salmonella Typhimurium. As of January 30, 2012, investigators collected antibiotic resistance information on isolates from 5 ill persons infected with the outbreak strain and on one of the leftover ground beef samples collected from an ill person’s home that yielded the outbreak strain. The isolate from the ground beef sample was resistant to multiple antibiotics, including amoxicillin/clavulanic acid, ampicillin, ceftriaxone, cefoxitin, kanamycin, streptomycin, sulfisoxazole, and tetracycline. The isolates from humans were also resistant to amoxicillin/clavulanic acid, ampicillin, ceftriaxone, cefoxitin, kanamycin, streptomycin, and sulfisoxazole; some were also resistant to tetracycline. All human isolates were sensitive to several common antibiotics used in clinical practice, such as ciprofloxacin, gentamicin, and trimethoprim-sulfamethoxazole. Antimicrobial resistance may increase the risk of hospitalization or possible treatment failure in infected individuals. Treatment decisions for individual patients should be guided by the results of antibiotic sensitivity testing performed on the specific Salmonella isolate from that individual.
Recall Information
On December 15, 2011, Hannaford, a Scarborough, Maine-based grocery chain, recalled an undetermined amount of fresh ground beef products that bear sell-by dates of December 17, 2011 or earlier.
Clinical Features/Signs and Symptoms
Most persons infected with Salmonella bacteria develop diarrhea, fever, and abdominal cramps 12 to 72 hours after infection. The illness usually lasts 4 to 7 days, and most persons recover without treatment. However, in some persons, the diarrhea may be so severe that the patient needs to be hospitalized. Salmonella infection may spread from the intestines to the bloodstream and then to other body sites and can cause death unless the person is treated promptly with antibiotics. Older adults, infants, and those with impaired immune systems are more likely to have a severe illness from Salmonella infection.
Advice to Consumers
This particular outbreak appears to be over. However, Salmonella is still an important cause of human illness in the United States. More information about Salmonella, and steps people can take to reduce their risk of infection, can be found on the CDC Salmonella Web Page and the CDC Vital Signs Web Page.
- Consumers should check their homes, including their freezers, for recalled ground beef products and not eat them; restaurant and food service operators should not serve it. Consumers with questions about recalled ground beef products may contact Hannaford’s Customer Information Center, 8 a.m. to 8 p.m. at telephone number (800) 213-9040, and choose option 6.
- Wash hands, kitchen work surfaces, and utensils with soap and water immediately after they have been in contact with raw meat or poultry, including frozen and fresh ground beef. Then, disinfect the food contact surfaces using a freshly prepared solution of 1 tablespoon unscented liquid chlorine bleach to 1 gallon of water.
- Cook ground beef thoroughly. Ground beef dishes should always be cooked to 160°F internal temperature as measured with a food thermometer; leftovers also should be reheated to 160°F. The color of cooked ground beef is not an indicator that product has been safely cooked. Only by using a food thermometer can one accurately determine that ground beef has reached a safe minimum internal temperature of 160°F throughout the product. Ground beef can remain pink even after cooking to a safe minimum internal temperature of 160°F. Be particularly careful with foods prepared for infants, older adults, and persons with impaired immune systems.
- If served undercooked ground beef in a restaurant, send it back to the kitchen for further cooking.
- Avoid cross-contaminating other foods. Uncooked meats and ground beef should be kept separate from produce, cooked foods, and ready-to-eat foods. Do not wash raw meat or poultry before cooking because splashing water can spread any pathogens present on raw meat surfaces to other kitchen surfaces. Hands, cutting boards, counters, knives, and other utensils should be washed thoroughly after touching uncooked foods. Hands should be washed before handling food, and between handling different food items.
- Refrigerate raw and cooked meat and poultry within 2 hours after purchase (1 hour if temperatures exceed 90°F). Refrigerate cooked meat and poultry within 2 hours after cooking. Refrigerators should be set to maintain a temperature of 40°F or below.
- Persons who think they might have become ill from eating possibly contaminated ground beef should consult their health care providers. Infants, older adults, and persons with impaired immune systems are more likely than others to develop severe illness.
Additional Resources
- FoodSafety.gov
- FSIS Fact Sheet on Meat Preparation: Ground Beef and Food Safety
- AskKaren.gov (FSIS virtual representative)
- 1-888-MPHotline (1-888-674-6854), USDA English/Spanish Meat and Poultry Hotline
CDC’s Role in Food Safety
As an agency within the U.S. Department of Health and Human Services (HHS), CDC leads federal efforts to gather data on foodborne illnesses, investigate foodborne illnesses and outbreaks, and monitor the effectiveness of prevention and control efforts. CDC is not a food safety regulatory agency but works closely with the food safety regulatory agencies, in particular with HHS’s U.S. Food and Drug Administration (FDA) and the Food Safety and Inspection Service within the United States Department of Agriculture (USDA). CDC also plays a key role in building state and local health department epidemiology, laboratory, and environmental health capacity to support foodborne disease surveillance and outbreak response. Notably, CDC data can be used to help document the effectiveness of regulatory interventions.
Final Case Count Map
Persons infected with the outbreak strain of Salmonella Typhimurium, by state, as of January 30, 2012 (n=20)
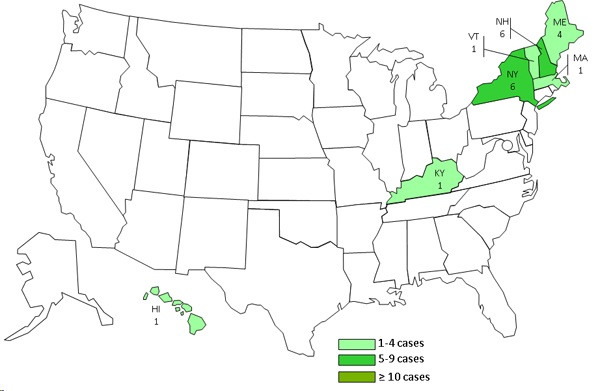
A total of 20 persons infected with the outbreak strain of Salmonella Typhimurium have been reported from 7 states. The number of ill persons identified in each state is as follows: HI (1), KY (1), MA (1), ME (4), NH (6), NY (6), and VT (1).
Final Epi Curve
Persons infected with the outbreak strain of Salmonella Typhimurium, by date of illness onset*
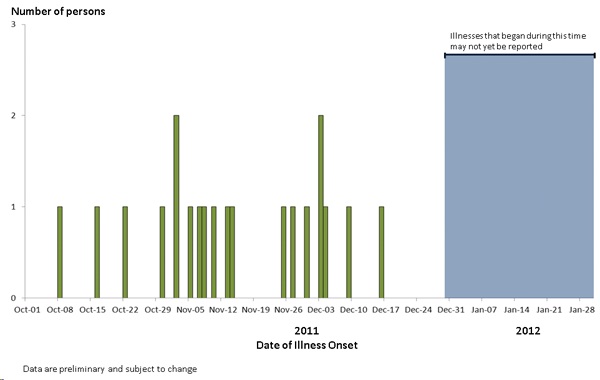
*n=20 for whom information was reported as of January 30, 2012