2015 Salmonella Outbreak Linked to JEM Raw Brand Sprouted Nut Butter Spreads
Posted January 15, 2016 3:15 PM ET
This outbreak appears to be over. However, the recalled nut butter spreads have a long shelf life and may still be in people’s homes. Consumers unaware of the recall could continue to eat the products and potentially get sick. Read the Advice to Consumers.
- This outbreak appears to be over. However, the recalled nut butter spreads have a long shelf life and may still be in people’s homes. Consumers unaware of the recall could continue to eat the products and potentially get sick. Read the Advice to Consumers.
- CDC collaborated with public health officials in multiple states and the U.S. Food and Drug Administration (FDA) to investigate a multistate outbreak of Salmonella Paratyphi B variant L(+) tartrate(+) infections.
- Thirteen people infected with the outbreak strain of Salmonella Paratyphi B variant L(+) tartrate(+) were reported from 10 states.
- No one was hospitalized, and no deaths were reported.
- This outbreak was caused by Salmonella Paratyphi B variant L(+) tartrate(+) bacteria, formerly known as Salmonella Java.
- People with illness caused by this bacteria typically experience diarrhea, fever, and abdominal cramps 12-72 hours after an exposure.
- Salmonella Paratyphi B variant L(+) tartrate(+) does not cause paratyphoid fever, enteric fever, or typhoid fever.
- The epidemiologic evidence collected during the investigation indicated that JEM Raw brand sprouted nut butter spreads were the likely source of this outbreak.
- All 10 ill people interviewed (100%) reported exposure to a nut butter or nut butter spread in the week before illness onset, and eight (80%) of these people specifically reported exposure to a JEM Raw brand sprouted nut butter spread.
- On December 2, 2015, JEM Raw Chocolate, LLC voluntarily recalled its entire line of sprouted nut butter spreads because of potential contamination with Salmonella.
- The recall affects all flavors of nut butter spreads sold by JEM Raw with best by dates of October 30, 2016 or earlier. The best by date can be found on the bottom of the jar.
- The nut butter spreads were distributed nationwide in retail stores and through mail order.
- The products were sold in glass jars in sizes ranging from 1.25 ounces to 16 ounces.
- CDC recommends that consumers, restaurants, and retailers do not eat, serve, or sell any of the recalled sprouted nut butter spreads.
- The nut butter spreads have a long shelf life.
- Any remaining nut butter spread should be thrown away. Even if some of the nut butter spread has been eaten and no one has gotten sick, the rest of it should be thrown away.
- Consumers can contact JEM Raw with questions about product replacement.
Introduction
CDC collaborated with public health officials in multiple states and the U.S. Food and Drug Administration (FDA) to investigate a multistate outbreak of Salmonella Paratyphi B variant L(+) tartrate(+) infections.
This outbreak was caused by Salmonella Paratyphi B variant L(+) tartrate(+) bacteria, formerly known as Salmonella Java. People with illness caused by this bacteria typically experience diarrhea, fever, and abdominal cramps 12-72 hours after an exposure. Salmonella Paratyphi B variant L(+) tartrate(+) does not cause paratyphoid fever, enteric fever, or typhoid fever.
Public health investigators used the PulseNet system to identify illnesses that may be part of this outbreak. PulseNet, the national subtyping network of public health and food regulatory agency laboratories, is coordinated by CDC. DNA “fingerprinting” is performed on Salmonella bacteria isolated from ill people by using a technique called pulsed-field gel electrophoresis, or PFGE. PulseNet manages a national database of these DNA fingerprints to identify possible outbreaks. One DNA fingerprint (outbreak strain) was included in this outbreak investigation. The outbreak strain was new to the PulseNet database.
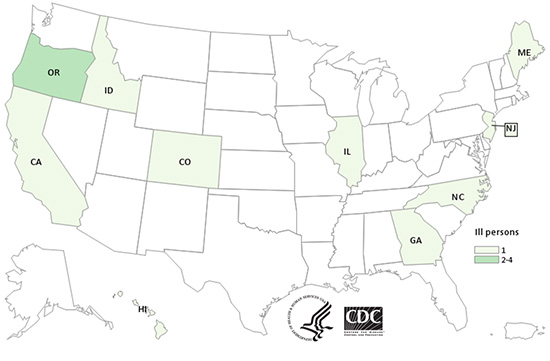
A total of 13 people infected with the outbreak strain of Salmonella Paratyphi B variant L(+) tartrate(+) were reported from 10 states. The number of ill people identified in each state was as follows: California (1), Colorado (1), Georgia (1), Hawaii (1), Idaho (1), Illinois (1), Maine (1), New Jersey (1), North Carolina (1), and Oregon (4).
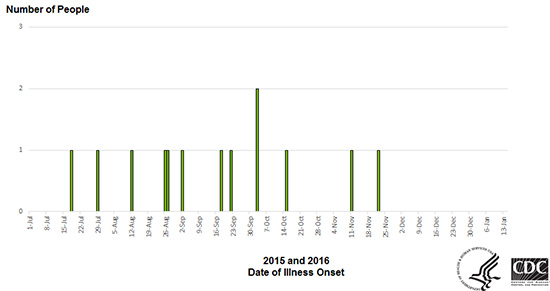
Illnesses started on dates ranging from July 18, 2015, to November 22, 2015. Ill people ranged in age from less than 1 year to 79, with a median age of 41. Sixty-two percent of ill people were male. Among 11 ill people with available information, none were hospitalized, and no deaths were reported.
This outbreak appears to be over. However, the recalled nut butter products have a long shelf life and may still be in people’s homes. Consumers unaware of the recall could continue to eat the products and potentially get sick.
Investigation of the Outbreak
The epidemiologic evidence collected during the investigation indicated that JEM Raw brand sprouted nut butter spreads was the likely source of this outbreak.
In interviews, ill people answered questions about foods eaten and other exposures in the week before they became ill. All 10 ill people interviewed (100%) reported exposure to a nut butter or nut butter spread in the week before illness onset, and eight (80%) of these people specifically reported exposure to a JEM Raw brand sprouted nut spread.
On December 2, 2015, JEM Raw Chocolate, LLC of Bend, Oregon, voluntarily recalled its entire line of sprouted nut butter spreads because of potential contamination with Salmonella. The recall affects all flavors of sprouted nut butter spreads sold by JEM Raw with best by dates of October 30, 2016 or earlier. The nut butter spreads were distributed nationwide in retail stores and through mail order. The products were sold in glass jars in sizes ranging from 1.25 ounces to 16 ounces.
The National Antimicrobial Resistance Monitoring System (NARMS) is a U.S. public health surveillance system that tracks antibiotic resistance in foodborne and other enteric bacteria found in people, raw meat, and poultry, and food-producing animals. NARMS is a partnership among the CDC, the U.S. Food and Drug Administration (FDA), USDA, and state and local health departments.
The NARMS human surveillance program at CDC monitors antibiotic resistance in Salmonella and other bacteria isolated from clinical specimens submitted to NARMS by public health laboratories. CDC’s NARMS laboratory conducted antibiotic resistance testing on clinical isolates collected from four ill people infected with the outbreak strain. All four isolates (100%) were susceptible to all antibiotics tested on the NARMS panel.