2015 Salmonella Outbreak Linked to Live Poultry in Backyard Flocks
Posted September 24, 2015 4:15 PM ET
These investigations are over. However, live poultry, including those kept in backyard flocks, remain an important cause of human Salmonella infections in the United States. More information about Salmonella from live poultry and the steps people can take to reduce their risk of infection is available.
- Read the Advice to Backyard Flock Owners »
- These investigations are over. However, live poultry, including those kept in backyard flocks, remain an important source of human Salmonella infections in the United States.
- Backyard flock owners should take steps to protect themselves and their families:
- Always wash hands thoroughly with soap and water right after touching live poultry or anything in the area where the birds live and roam.
- Do not let live poultry inside the house.
- Learn about additional recommendations to prevent Salmonella infections from live poultry. These recommendations are important and apply to all live poultry, regardless of the age of the birds or where they were purchased.
- Mail-order hatcheries, agricultural feed stores, and others that sell or display chicks, ducklings, and other live poultry should provide health-related information to owners and potential purchasers of these birds prior to the point of purchase. This should include information about the risk of acquiring a Salmonella infection from contact with live poultry.
- CDC, public health, veterinary, and agriculture officials in many states and the U.S. Department of Agriculture’s Animal and Plant Health Inspection Service (USDA-APHIS) investigated four multistate outbreaks of human Salmonella infections linked to contact with live poultry.
- 252 people infected with the outbreak strains of Salmonella were reported from 43 states.
- 63 ill people were hospitalized, and no deaths were reported.
- Epidemiologic, laboratory, and traceback findings linked these four outbreaks of human Salmonella infections to contact with chicks, ducklings, and other live poultry from multiple hatcheries.
- 146 (80%) of the 183 ill people who were interviewed reported contact with live poultry in the week before their illness began.
- CDC’s National Antimicrobial Resistance Monitoring System (NARMS) laboratory conducted antibiotic resistance testing on Salmonella isolates collected from 20 ill people infected with one of the outbreak strains.
- 19 (95%) isolates were susceptible to all antibiotics tested on the NARMS panel.
- One (5%) isolate was resistant to sulfisoxazole.
Introduction
CDC collaborated with public health, veterinary, and agriculture officials in many states and with the U.S. Department of Agriculture’s Animal and Plant Health Inspection Service (USDA-APHIS) to investigate four multistate outbreaks of human Salmonella infections. Results from these investigations indicated that contact with live poultry was the likely source of these outbreaks.
Public health investigators used the PulseNet system to identify illnesses that were part of these outbreaks. PulseNet is the national subtyping network of public health and food regulatory agency laboratories coordinated by CDC. DNA “fingerprinting” is performed on Salmonella bacteria isolated from ill people by using a technique called pulsed-field gel electrophoresis, or PFGE. PulseNet manages a national database of these DNA fingerprints to identify possible outbreaks. A total of 10 DNA fingerprints (“outbreak strains”) were included in these investigations.
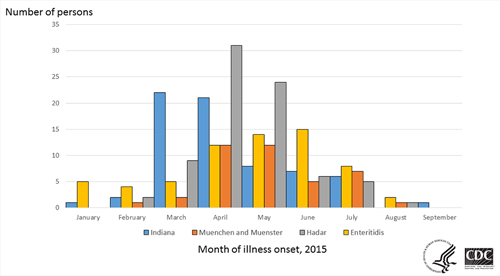
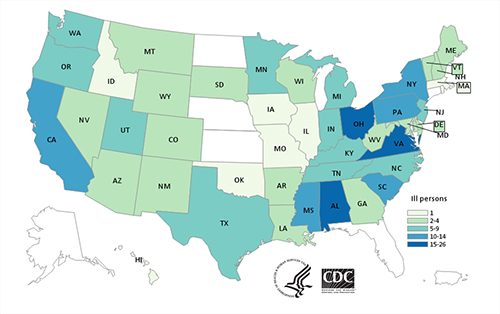
In the four outbreaks, 252 people infected with one of the outbreak strains of Salmonella were reported from 43 states between January 3, 2015 and September 6, 2015.
Investigation of the Outbreaks
In interviews, ill people answered questions about contact with animals and foods consumed during the week before becoming ill; 146 (80%) of the 183 ill people interviewed reported contact with live poultry (e.g., chicks, chickens, ducks, ducklings) before becoming ill. Ninety-four ill people who had purchase records available reported purchasing live baby poultry from 41 different suppliers, including feed supply stores, Co-Ops, “flea markets”, friends, and hatcheries in multiple states. Ill people reported purchasing live poultry for backyard flocks to produce eggs or meat or to keep as pets. Twenty-eight (41%) of 69 ill people with complete questionnaires reported keeping baby poultry indoors, 39 (57%) of 69 reported holding or snuggling baby poultry, and 4 (6%) of 69 reported kissing baby poultry. These behaviors increase a person’s risk of a Salmonella infection.
CDC’s National Antibiotic Resistance Monitoring System (NARMS) laboratory conducted antibiotic resistance testing on clinical isolates collected from 20 people infected with one of the outbreak strains. One (5%) isolate was resistant to sulfisoxazole, and 19 (95%) isolates were susceptible to all antibiotics tested on the NARMS panel.
Final summaries of the four outbreak investigations are provided below.
Outbreak 1: Salmonella Enteritidis Investigation
Sixty-five people infected with the outbreak strains of Salmonella Enteritidis were reported from 18 states. The number of people in each state was as follows: Arizona (1), California (3), Georgia (1), Indiana (1), Maine (1), Minnesota (7), New Hampshire (3), Ohio (20), Oklahoma (1), Oregon (3), South Carolina (2), Tennessee (1), Texas (2), Utah (5), Vermont (2), Virginia (7), Washington (4), and Wyoming (1).
Illness onset dates ranged from January 3, 2015 to August 4, 2015. Ill people ranged in age from younger than one year to 81, and the median age was 32. Fifty-two percent of ill people were male. Among 50 ill people with available information, 12 (24%) were hospitalized, and no deaths were reported.
Outbreak 2: Salmonella Hadar Investigation
Seventy-eight people infected with the outbreak strains of Salmonella Hadar were reported from 30 states. The number of people in each state was as follows: Arizona (2), Arkansas (2), California (3), Colorado (1), Delaware (2), Iowa (1), Kentucky (1), Louisiana (2), Maine (1), Maryland (3), Massachusetts (1), Michigan (1), Minnesota (1), Missouri (1), Montana (4), North Carolina (2), New Jersey (2), New Mexico (1), New York (3), Ohio (3), Oregon (5), Pennsylvania (11), South Carolina (4), South Dakota (2), Texas (2), Virginia (8), Washington (4), West Virginia (1), Wisconsin (1), Wyoming (3).
Illness onset dates ranged from February 22, 2015 to August 26, 2015. Ill people ranged in age from younger than one year to 89, and the median age was 39. Fifty-two percent of ill people were female. Among 51 ill people with available information, 29 (57 %) were hospitalized, and no deaths were reported.
Outbreak 3: Salmonella Indiana Investigation
Sixty-eight people infected with the outbreak strains of Salmonella Indiana were reported from 18 states. The number of people in each state was as follows: Alabama (17), Arkansas (2), California (5), Colorado (1), Georgia (2), Idaho (1), Maryland (1), Mississippi (13), Nevada (4), New Jersey (2), New Mexico (1), New York (8), North Carolina (1), Oregon (1), Pennsylvania (1), South Carolina (6), Tennessee (1), and Texas (1).
Illness onset dates ranged from January 6, 2015 to September 6, 2015. Ill people ranged in age from younger than one year to 89, and the median age was 2. Fifty-three percent of ill people were female. Among 39 ill people with available information, 12 (31 %) were hospitalized, and no deaths were reported.
Outbreak 4: Salmonella Muenchen and Salmonella Muenster Investigation
Forty-one people infected with the outbreak strains of Salmonella Muenchen or Salmonella Muenster were reported from 19 states. The number of people in each state was as follows: Alabama (3), California (1), Georgia (1), Hawaii (1), Illinois (1), Indiana (4), Kentucky (4), Michigan (5), New Jersey (2), New York (1), North Carolina (2), Ohio (3), Pennsylvania (1), Tennessee (5), Utah (1), Virginia (1), Washington (1), West Virginia (3), and Wisconsin (1).
Illness onset dates ranged from February 26, 2015 to August 10, 2015. Ill people ranged in age from younger than one year to 77, and the median age was 18. Fifty-six percent of ill people were male. Among 30 ill people with available information, 10 (33 %) were hospitalized, and no deaths were reported.